Published on .
Medication adherence is critically important for both Star Ratings and positive health outcomes for members. How can health plans empower their members to become adherent (and stay adherent) to their medications?
For health plans, helping members achieve and sustain medication adherence is a critical goal – and an ongoing public health challenge.
Health plans know how important it is for their members to remain adherent to their medication regimens. Plans that wish to score well on the Star Ratings scale must meet stringent adherence measures that comprise approximately one-third of their overall Star Ratings results and directly impact overall plan performance.
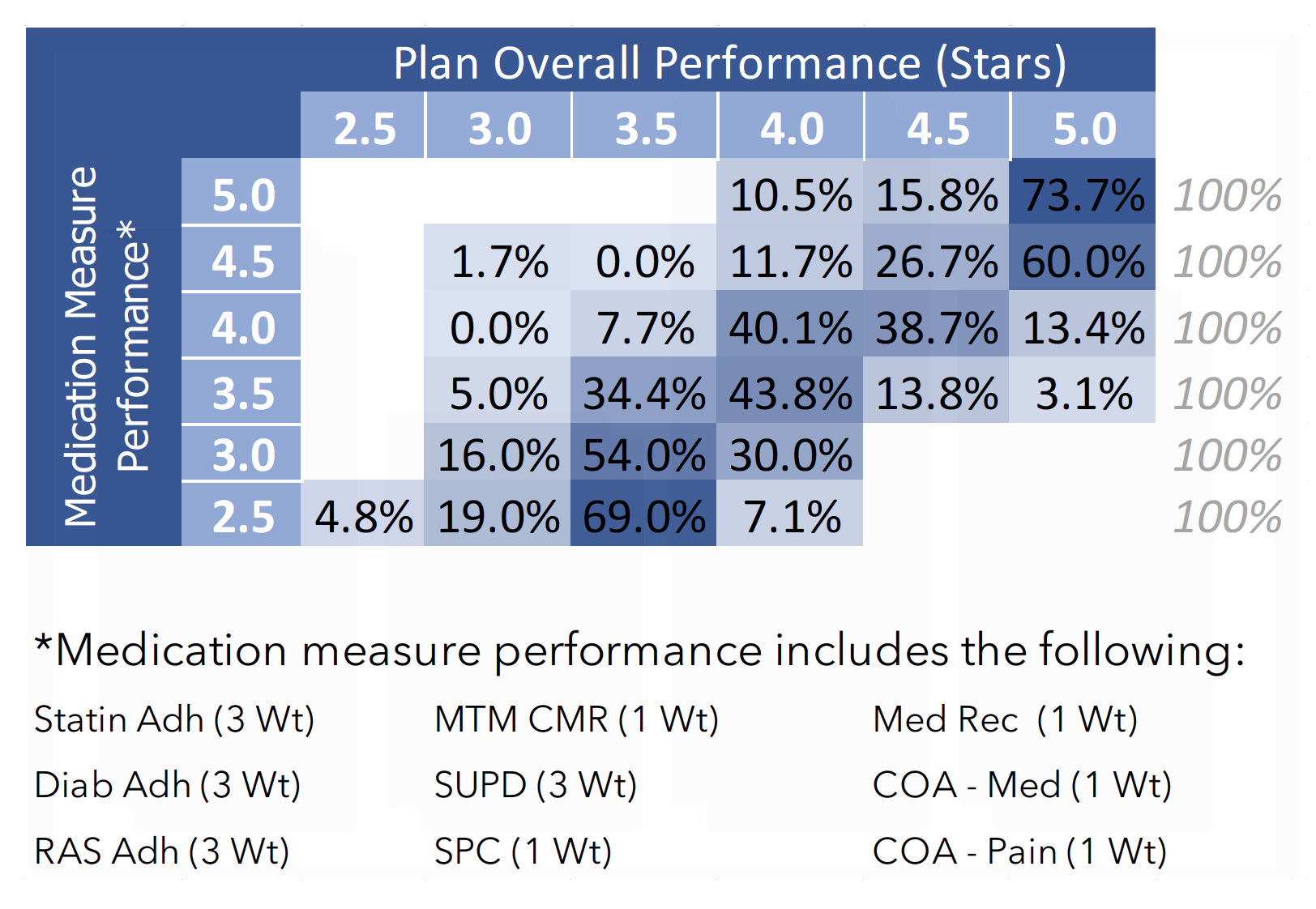
Poor performance on crucial medication adherence measures actively dragged down Star Rating scores for health plans in the 2022 Star Ratings year. An AdhereHealth analysis showed that plans achieving 4.5 and 5 Stars on medication measures were much more likely to achieve 5 Stars in overall plan performance.
On top of that, medication adherence is directly tied to reductions in spending and better long-term health outcomes, particularly for members living with chronic diseases. For example, a 2021 report from CMS estimates that improved medication adherence for Medicare beneficiaries with diabetes, hypertension, and high cholesterol saved between $27 and $46.6 billion between 2013 and 2018.
The increased focus on medication management, including comprehensive medication reconciliation and adherence activities, has also helped to narrow ethnic, racial, and socioeconomic disparities in the ability to access and correctly utilize medications.
Unfortunately, achieving medication adherence among members with elevated clinical risks and complex socioeconomic circumstances isn’t always easy. These members often face financial and behavioral barriers to adherence that prevent them from consistently taking their prescriptions as directed.
To boost performance on medication adherence measures and set members up for successful self-management, health plans will need to engage in proactive, holistic strategies to address the roots of medication nonadherence and offer meaningful, personalized support to their highest risk members.
Here are the top 4 real-world strategies for improving medication adherence rates among the hardest-to-reach populations.
Get ahead of the gaps with timely and effective touchpoints
The Star Ratings medication adherence metrics rely on a calculation of the percentage of days covered (PDC), or how many days out of the previous year the member had access to their medications.
But there are two major problems with this formula. For one thing, having access to medications is not equivalent to having taken the medications as instructed.
And secondly, by the time the health plan is aware that the member is falling short, it may already be too late. The member will likely fall short of the required PDC to qualify as adherent for Star Ratings during that performance year, and there’s no going back in time to fix the problem.
Health plans can’t afford to wait for several months until they get information that the member hasn’t been keeping up with their prescriptions. Instead, they need to invest in analytics tools that flag potentially non-adherent members before the measurement period is too far gone. Then, they must design proactive, effective outreach schedules to keep members on the right path.
These timely touchpoints should start during the first quarter of the year. Reaching out to these members as early as possible will give health plans the best chance of catching and closing gaps before they form.
Make socioeconomically sensitive motivational interviewing a core competency
Members with medication adherence issues typically have several different financial, functional, and behavioral issues that make everyday life a challenge. Health plans cannot expect that a text message reminder will offer the support, understanding, and personalized problem-solving that these members need to develop healthier habits.
Instead, plans should incorporate motivational interviewing techniques that get to the heart of the individual’s barriers and concerns. By combining open-ended, non-judgmental questions about behavior with patient education and referrals to community-based resources, motivational interviewing makes members feel respected, heard, and empowered to make positive changes.
During these conversations, outreach staff shouldn’t just talk about clinical matters. Socioeconomic barriers, such as food and housing insecurity, low health literacy, and lack of transportation may have an even bigger impact on medication adherence than the undesirable side effects of a particular drug.
Outreach staff must have the ability to connect members to local resources that can solve for these problems, giving members a better chance of building good habits and a better life.
Leverage the benefits of compliance packaging and medication synchronization
Health plans have a number of tools at their disposal to make medication access easier and less complicated, particularly among members with eight or more prescriptions. Chief among these are compliance packaging and medication synchronization.
Compliance packaging can provide a major boost to members with multiple medications or frequent dosing requirements. These color-coded pill packs or strips, with doses organized by date and time, make it simple for members to take control of their routines.
In conjunction with clear packaging, health plans can arrange medication synchronization so members only have to make one trip to the pharmacy (or receive in-home delivery) to collect all of their prescriptions. Medication synchronization can be very helpful for individuals with transportation issues, including people living in one of the many pharmacy deserts in urban and rural areas across the country.
Invest in kindness as members build better relationships with their medications
All these activities must combine in an intentional way to provide compassionate, trustworthy support for members seeking to build more positive relationships with their own self-care.
Health plans must remember that individuals from all walks of life may feel overwhelmed, angry, suspicious, patronized, or helpless when it comes to interactions with the healthcare system, especially if they are struggling to cope with poor health on a regular basis.
Kindness and patience are just as important as clinical experience and community-based resources to help members make long-term changes to their behaviors. Health plans should prepare to invest time and effort in their high-risk members (an effective motivational interviewing session may take up to 20 minutes) and arrange for frequent check-ins to ensure that each person is able to stay on track with their journey toward medication adherence.
Health plans only have a fragile window of time to create the conditions for optimal medication adherence. With proactive outreach, motivational conversations, smart medication management tools, and a personalized touch, health plans can successfully foster better outcomes for members while securing higher Star Ratings.
For more insights about improving adherence, subscribe to our blog to receive updates as soon as they’re available.
