Published on .
Data is powerful. And the ability of health plans and other entities to leverage data to drive improved medication adherence for high-risk members is critical to successful plan performance, improved member health outcomes and satisfaction, and increased health equity.

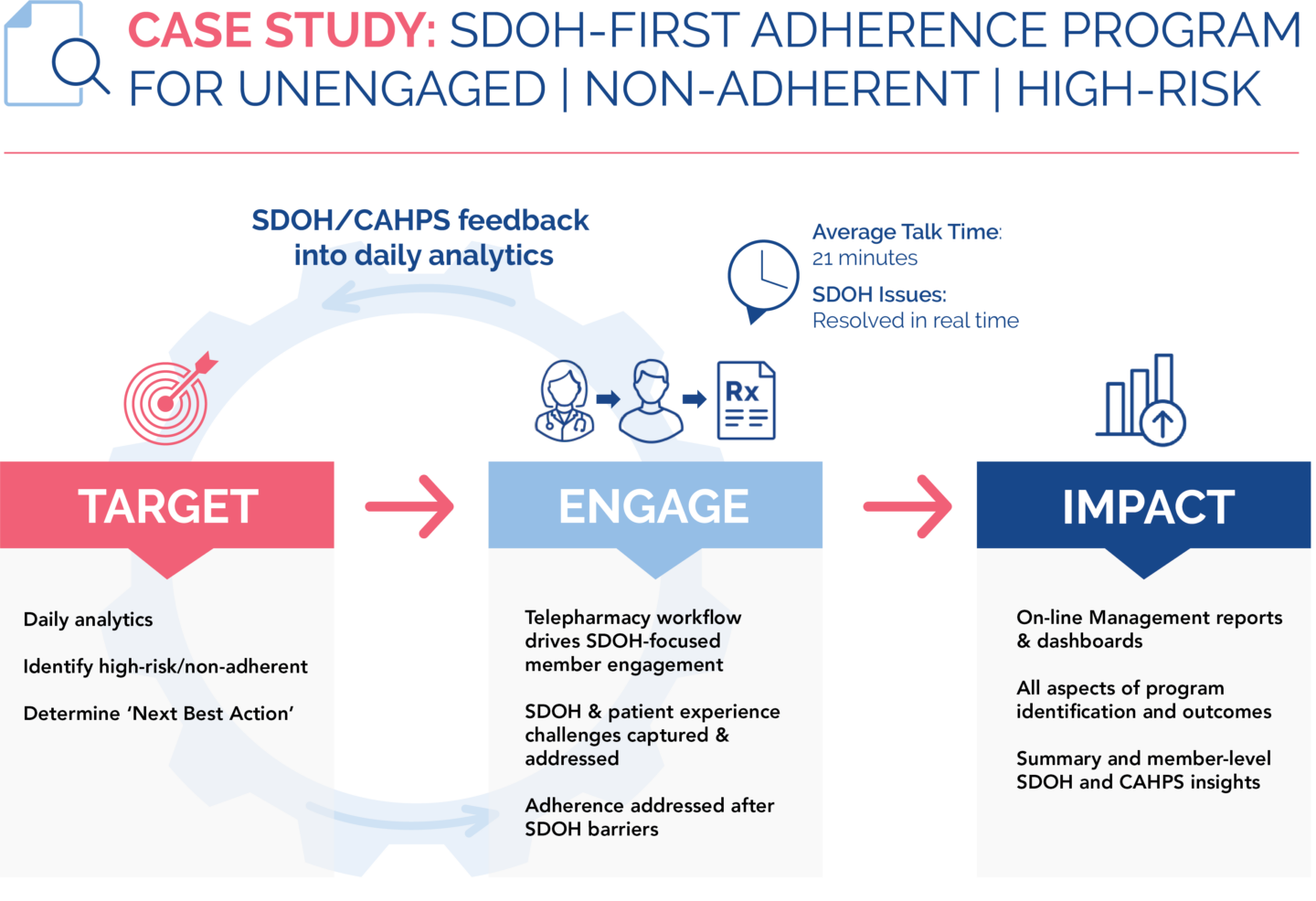
With the right technology platform (in the form of “Software as a Service,” or SaaS) underlying clinician outreach and engagement efforts, plans can maximize identification of and support for at-risk members in need of intervention and support.
This technology is most effective when it helps address issues with social determinants of health (SDOH), or the circumstances in which people live, work, grow and age.
SDOH barriers (which may include food and housing insecurity, health illiteracy, loneliness and lack of transportation access) are changing what it means to be a “high-risk” health plan member or patient, and consist of direct obstacles in the way of a person staying adherent with a medication, treatment schedule or general health recommendations.
The growing need for health equity in healthcare
A huge proportion of the American public faces one or more SDOH barriers. Some of these, such as racial or gender discrimination, polluted air and water, and limited economic opportunities, are beyond the scope of any one industry’s realm of influence; therefore, comprehensive, lasting solutions require multi-disciplinary strategies that intertwine multiple support networks. Within this context, specific socioeconomic factors, such as access to nutritious food, affordable medication, health-related education and transportation to medical appointments, are more in scope for health plans and clinicians to address within their communities. And by helping members overcome these barriers to care, they can improve health outcomes and, in turn, health equity.
There are powerful incentives for committing to the investment. SDOHs are commonly thought to impact up to 80% of overall health outcomes, thereby representing a critical fulcrum for improving member experiences, boosting long-term outcomes—and securing immediate benefits from improved performance on important performance metrics, such as the Star Ratings system.
Taking action on SDOH barriers and health equity through technology
When clinician intervention is supported by strong, data-driven technology, plans can develop and maintain meaningful relationships with the highest-risk, highest-complexity plan members, whose significant clinical challenges may be exacerbated by SDOH barriers. Reinforced by proper communication with provider and pharmacy networks, these SaaS-enabled clinician-to-member relationships form the foundation of better outcomes for individuals and higher performance for plans on critical performance programs that help these plans remain competitive in a pressure-filled environment.
But not all platforms are created equal, and it’s important to select a solution with robust and effective features, including the ability to maximize identification of high-risk members; track outreach; manage member, provider, and pharmacy engagement; close the loop on SDOH referrals; and monitor adherence to recommended treatments and services.
Leveraging data-driven, SaaS solutions to establish and maintain relationships with high-risk individuals
Making a difference in a member’s life starts by establishing trust, building a relationship and providing reliable, ongoing support for that person on a long-term basis. To do this at scale, health plans and other entities can harness the power of a true patient relationship management (PRM) solution to identify and stratify members for engagement, guide outreach workflows, and ensure documentation of efforts for internal communication and care coordination.
 Top five capabilities of a robust data-driven platform
Top five capabilities of a robust data-driven platform
- Align multisource data for holistic understanding of member needs. Getting to the heart of SDOH barriers requires a platform that starts the process by using rich, multi-source data (including clinical data, claims and socioeconomic data such as the CDC Social Vulnerability Index) to stratify populations by risk and prioritize specific individuals for outreach. It’s most effective if the platform runs analytics daily to deliver the most accurate and up-to-date information to clinicians every morning for outreach. This helps a plan maximize the identification of high-risk members in need of clinician outreach and support, for improved health outcomes, as well as cost savings through avoidance of future medical services.
- Recommend the “next best action” for the most effective clinician support. An ideal platform can then prompt clinicians to take the next best action for the member, such as activating an unused transportation benefit for medical appointments or connecting the person with a local food pantry providing fresh and nutritious options. This built-in guidance helps drive the most effective SDOH-focused workflow, ensuring all member needs are captured and addressed.
- Track member information and conversation details to avoid abrasion. Once outreach professionals have data on who to contact, they need to understand the health plan’s history with that member and where that person is in their health journey. While many technology options on the market are focused on generating prioritized lists for member outreach, most don’t go far enough with capabilities to track those members over time to help ensure long-term adherence, without the abrasion of having to ask the person the same sensitive questions over and over. Technology tools should be able to ingest information gathered from members and their providers during previous phone calls and interactions, and surface those notes to users in an intuitive and easy-to-understand manner, integrating them back into the daily platform analytics to support clinician outreach. This longitudinal record-keeping can foster seamless, personalized relationships that help clinicians support members in resolving SDOH barriers and reflect how much the health plan truly cares about their members and their experiences.
- Connect members to community resources in real time. A platform that surfaces potential resources to share with members immediately during a conversation helps ensure SDOH barriers aren’t just identified: they are actually resolved quickly. Closing the loop helps members while equipping health plans, providers, and other entities with the data they need to learn from these interactions, design high-impact, holistic, person-centered interventions that support members in the long term, continuously improve performance on Stars and other P4P measurement systems.
- Generate summaries and reports to monitor plan performance. For insight into plan performance, it helps when platforms generate summaries and reports, detailing member interactions and outcomes for insight into SDOH trends across the health plan. Self-service dashboard visualization portals are also an intuitive and easy-to-use way to access and review key SDOH engagement details and themes, at the patient and population levels.
The right technology platform can become the foundation of success for health plans operating in a marketplace where there is no room for error, particularly with challenges like medication adherence and its wide-ranging impacts on financial, clinical and member experience goals.
As SDOHs and health equity continue to be a major focus across the entire care continuum, health plans and other entities need to invest in the technologies and strategies required to identify high-risk, high-complexity members and address their non-clinical challenges in a personalized and coordinated manner.
In need of a SaaS solution to support your health plan’s clinician outreach and engagement? Contact AdhereHealth to discover how our proprietary healthcare technology platform helps you harness the power of data to drive SDOH resolution, adherence improvements and optimum plan performance.
 Authored by:
Authored by:
Kempton Presley, MPH, MS
AdhereHealth Chief Analytics Officer
