Published on .
The PP2 results were concerning, if not alarming, for many MA plans. And now, with the subsequent release of the 2024 Star Ratings from CMS, it’s important for plans to note that your Star Rating may be in the books, but your future performance is in your hands!
Continuing our annual fall webinar series, AdhereHealth panelists were recently joined by Mick Twomey, CEO of Hyperlift, for the first of three webinars to discuss insights and key areas of focus for the CMS Star Ratings. We caught back up with Mick afterwards to reflect on what plans may be experiencing with the massive changes revealed in the 2024 results, and what plans can do to prepare for success in the 2024 measurement year.
1. How did the Tukey method impact the Stars cut points, and which were the most impacted?
This is the most impactful change we’ve seen to date from CMS to the Star Ratings. And though it may feel shocking, I think now that Tukey is out and it’s real, many plans have experienced impacts they hopefully were expecting when this change was first announced.
The Tukey outlier method tends to have more of an impact on the lower end of the Star Ratings cut points (2- and 3-Star cut points) than it does on the higher end. However, it really did have a big impact on 2024, even at the higher end of the cut points in contracts where you might think they’d be more immune to the impact of Tukey. By removing the lower outliers, it has the potential to markedly increase the cut points we are used to.
From Stars 2023 to Stars 2024, seven measures saw cut point increases of over 20 basis points, with two experiencing cut point changes of 20 basis points in at least two cut point bands.
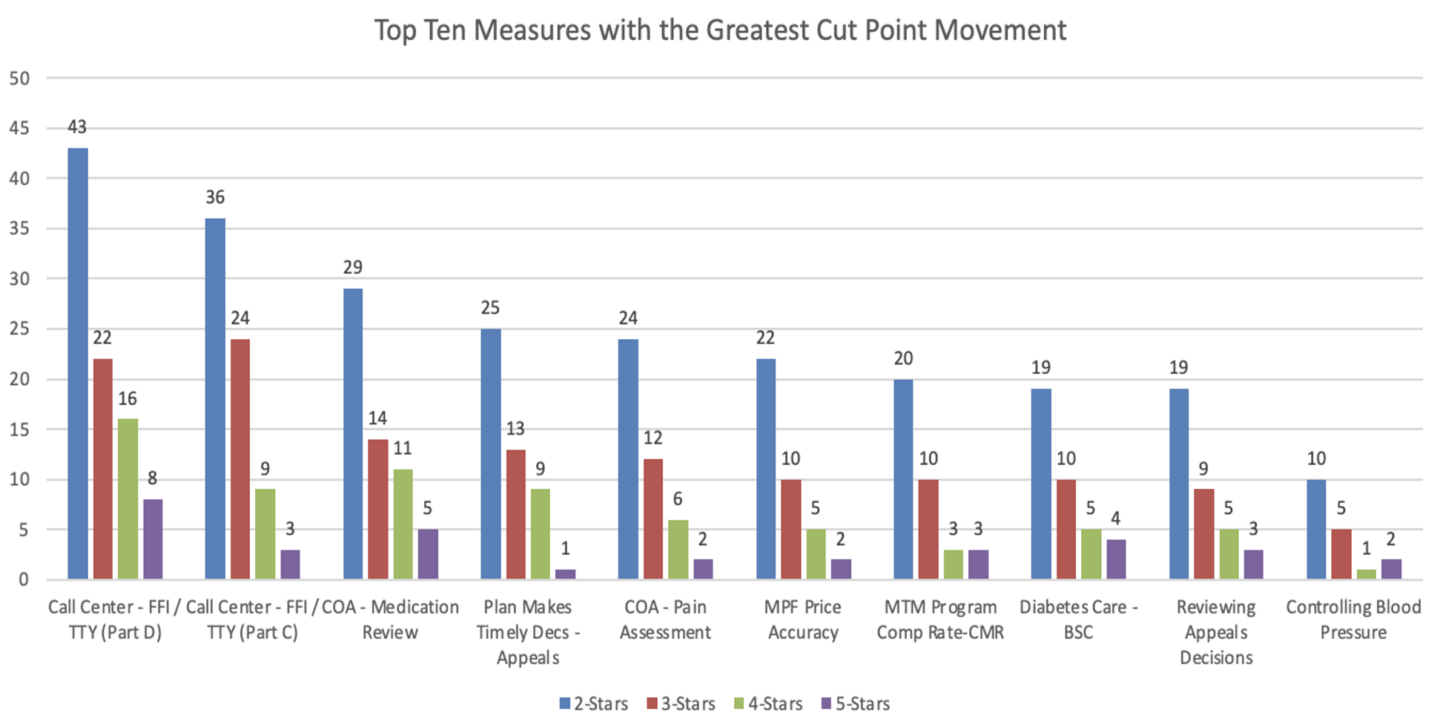
It can help plans prepare for future Star Ratings impact by operating with these new cut points in mind, and a solid Stars strategy should include understanding where to place focus, based on the plan’s individual Stars performance, to get things back on track. This includes understanding the measures where your plan can “double down” to make the most impact on your overall Stars.
2. Are the guardrail ranges helpful for plans?
 There’s an impression that guardrails are a form of safety net so plans can better anticipate cut point projection trends. However, the stability offered by guard rails might have provided more projection for plans prior to the Tukey method being implemented. The whole purpose of Tukey is to move the cut points as the industry dictates based on overall performance. There was some misunderstanding that the guardrails would be applied to the actual 2023 cut points, but they were instead applied to the Tukey version of the Stars 2023 cut points. And this caused the cut points in some situations to jump higher than plans anticipated, and the 2024 Star Ratings were likely quite shocking for some. People had a false sense of security that guardrails were going to protect them, but in several situations, the guard rails kept the cut points from dropping more than they would have without them.
There’s an impression that guardrails are a form of safety net so plans can better anticipate cut point projection trends. However, the stability offered by guard rails might have provided more projection for plans prior to the Tukey method being implemented. The whole purpose of Tukey is to move the cut points as the industry dictates based on overall performance. There was some misunderstanding that the guardrails would be applied to the actual 2023 cut points, but they were instead applied to the Tukey version of the Stars 2023 cut points. And this caused the cut points in some situations to jump higher than plans anticipated, and the 2024 Star Ratings were likely quite shocking for some. People had a false sense of security that guardrails were going to protect them, but in several situations, the guard rails kept the cut points from dropping more than they would have without them.
Now with the cut points acting alongside Tukey, it’s entirely possible the guardrails may artificially inflate cut points in future years, because it’s more likely for the industry average to drop in a significant way (like during a pandemic) rather than to improve in a significant way.
3. The weighting of member experience measures is decreasing. What does this mean for plans?
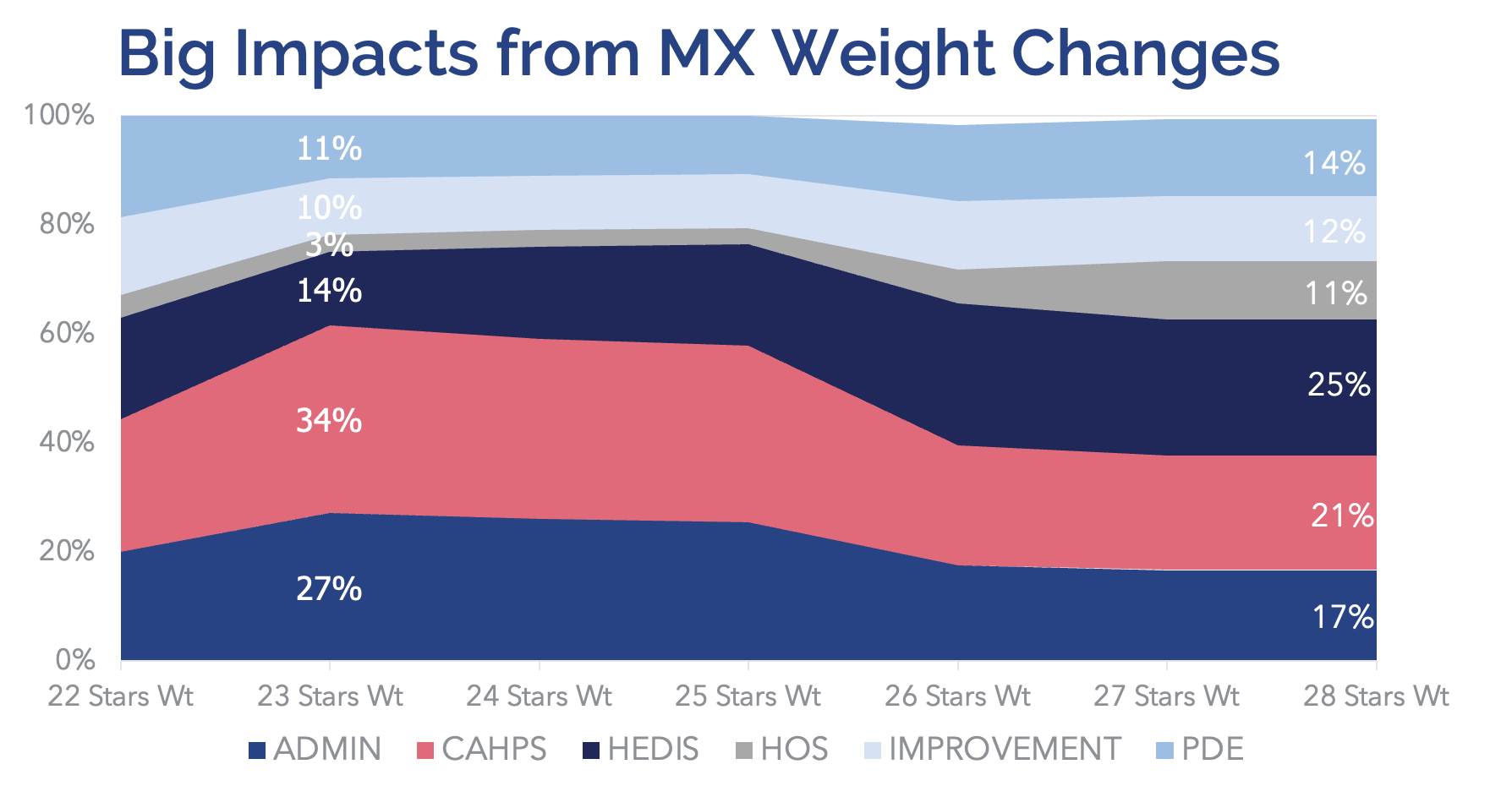
CMS had bumped the member experience measures up to a weight of 4, so in Stars 2023, member experience measures were the highest-weighted measures, accounting for right around 60% of a plan’s score. Now, with the finalized change to reduce member experience measure weighting back to down 2x for Stars 2026, HEDIS measures will become the highest-weighted group of measures (25% of the overall Star Rating), with pharmacy measures slated to account for 15%.
This impacts the way plans should think about their Stars math and where they need to apply additional focus. Member experience weights will still account for 40%, but with the reduced weight, plans will need to be cognizant about where they specifically need to focus efforts within the Stars strategy, especially with HEDIS and pharmacy measures now increasing in relative weight.
4. How will removal of the reward factor affect plans?
Depending on your plan’s performance, the removal of the reward factor might not matter at all to your plan, or it might be very scary. Because if you’ve been relying on 30 or 40 basis points each year to bump your score into a 4.5+ range, this is a fundamental change that will likely not be replaced with the Health Equity Index (HEI) bonus. That’s because plans currently receiving a high reward factor likely will not receive a high bonus from HEI since the membership mix that is often a factor in high performance won’t be the same one qualifying the plan for the HEI bonus. Even still, the HEI bonus won’t be a full replacement of the reward factor, as the average bonus from HEI is 11 basis points, while the average Reward Factor bonus was close to 30 basis points.
5. If our plan doesn’t currently have cohorts of SRF members, should we add this type of membership to get improved scoring from the HEI measure to receive the bonus?
A health plan that doesn’t currently offer capabilities to manage a membership facing social risk factors may initially struggle after adding such members, as this requires different processes and a different skill set. So, adding them for the sake of HEI is risky. However, for plans that do have SRF members, it is now more important than ever before to have strategies to address adherence performance for these cohorts.
6. Which types of plans fared well with all the challenges from CMS, when it seems like most plans fared poorly?
We do see a lot of risk coming up, but the plans that may have fared best could be the high-performing D-SNP plans. If you’re a high performing plan, you’re likely already comfortable understanding how to engage underserved populations facing social determinants of health (SDOH) factors that will be impacted by the HEI measure. These types of plans also may have never qualified for reward factor, so the removal of that wouldn’t matter, AND they’ll be well-positioned to earn the upcoming HEI bonus.
But despite how your plan fared, action is now everything. Understanding what measures will have the most impact on your overall Stars will be critical for forming a strategy to get started on improvements. And then implementing those improvement strategies will make all the difference in how your plan fares in future Stars, especially given all the changes that we’ve seen for 2024, and with other proposed changes looming ahead to be finalized by CMS.
Gain insight into the 2024 Star Ratings, plus strategies to take action for improvement. Join AdhereHealth at our upcoming webinar, the second in our 3-part series: Transforming Stars Scoring Shockwaves: Pivotal Strategies for Positive Impact on November 8. Register today: AdhereHealth – Industry Leading Technology Company

