Published on .
In PY 2021, many Medicare Advantage health plans struggled to meet all four components of the newly revamped Transitions of Care (TRC) Star Ratings measure, signaling challenges ahead as the metric goes live.
Medicare Advantage (MA) health plan members are at their most vulnerable during transitions of care. Transitions bring a number of risks, including the potential for critical health information to get lost in the shuffle.
A transition of care occurs any time a member moves from one care setting to another, such as from an inpatient bed to a skilled nursing facility or from the hospital back to their home.
Often, these events involve new diagnoses, additions or changes to medications, complex discharge instructions, or recommendations for follow-ups with primary care providers and specialists.
To ensure that members, providers, and health plans all have access to accurate, up-to-date clinical information, the MA Star Ratings system has introduced a new Transitions of Care (TRC) measure to enhance the existing medication reconciliation (MRP) metric. The updated requirements are more robust in that they include three additional components beyond MRP, including: notification of inpatient admission, receipt of discharge and patient engagement activities.
The three new components have been display measures for the past three years, allowing plans to ease into the new requirements. In other words, plans’ performance on inpatient and discharge notifications and patient engagement activities were being tracked and measured through performance year 2021, but that performance did not count toward their final Star Rating – until now. Unfortunately, preliminary results are not all plans could wish for.
Performance data for the display measure reveals that most health plans are falling short in at least one area of the four-part metric, and relatively few are hitting all the right notes to get full credit for their performance.
What happened during the demonstration year and how can MA plans improve their care coordination competencies to see better outcomes in 2022 and beyond?
Understanding the Makeup of the TRC Measure
The TRC measure comprises four interrelated tasks that add to the more familiar MRP metric of years past. The measure reviews the percentage of discharges that include all four indicators of a successful transition of care:
• Notification of inpatient admission: Documentation in the medical record of receipt of notification of inpatient admission on the day of admission or within the following 2 calendar days
• Receipt of discharge information: Documentation in the medical record of receipt of discharge information on the day of discharge or within the following 2 calendar days
• Patient engagement after inpatient discharge: Evidence of contact with the patient within 30 days of discharge, including an office visit, telehealth visit, or home visit
• Medication reconciliation post discharge: Medication reconciliation conducted on the date of discharge through 30 days after discharge (31 total days)
The new admission and discharge components are designed to help providers and health plans initiate medication reconciliation and patient engagement more quickly and consistently after a qualifying event.
Ideally, ensuring that all eligible members receive medication reconciliation services will reduce the sky-high readmission rates among the Medicare aged population. Currently, one in five Medicare beneficiaries will experience a 30-day readmission in any given year. Approximately a quarter of these readmissions are related to medication issues, such as patient non-adherence and dosing errors.
Analyzing MA Plan Performance on the TRC Demonstration Measure
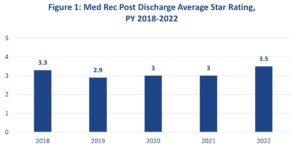
Source: CMS. Part C and D Performance Data. Star Ratings Fact Sheet, 2022 and 2021. Accessed February 28, 2022.
On the payer side, MA plans have historically exhibited poor performance on the MRP measure, averaging 3.1 out of five possible Stars since 2018 (Figure 1). And on the provider side, healthcare organizations are still finding it extremely difficult to send and receive data outside of their own integrated delivery systems.
Combining these two requirements into the MRP measure will inevitably pose problems for the MA plans now being held accountable for completing successful care transitions.
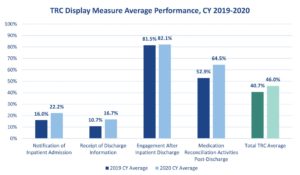
In February, CMS released its 2022 MA Star Ratings Display Measure Performance Data. An AdhereHealth analysis found that while more than 80 percent of plans, on average, conducted patient engagement after inpatient discharge, only a mere 22 percent were able to satisfy the requirement to send notifications of inpatient admission. And only 16.7 percent were able to acknowledge receipt of discharge information in CY 2020.
Even more concerning, the data showed that overall, just 46 percent of MA plans submitted data for all four categories of the TRC measure in PY 2020. The most successful plans were generally integrated provider/payer entities, which tend to experience the fewest obstacles with data exchange and continuity of care.
Source: CMS. Part C and D Performance Data. 2022 Display Measures Data. Accessed February 28, 2022.
This poor performance may spell trouble for health plans that have not yet focused on developing their medication reconciliation and interoperability competencies. In CY 2022, the measure will be single weighted within the Star Ratings system. However, TRC will become triple-weighted, if not more, in the coming years – adding even more pressure on health plans to get it right.
With the Star Ratings moving swiftly toward prioritizing member experiences and care coordination, plans will need to make sure they devote time and resources to monitoring member activities in real-time and conducting thorough medication reviews immediately after a utilization event.
How to Improve Performance on the TRC Measure
With the new structure, CMS is asking health plans to take greater control of the member experience. Health plans will need to immediately implement a coordinated, multi-pronged approach that involves stakeholders across the care continuum.
To succeed, plans must move past the basics of medication reconciliation. Instead of simply reviewing a record, MA plans should use a combination of experienced pharmacists and advanced analytics tools to proactively identify potential medication issues and address those issues holistically with members. Data-driven technology now enables plans to proactively monitor integrated data from medical and pharmacy claims to identify potential Drug Therapy Problems (DTP). Real-time intelligent insights can be delivered in existing clinicians’ workflows, whether via fax, letter, or medication reconciliation reports delivered to patients and physician offices, creating an omnichannel approach to maximize completion rates.
For many MA beneficiaries, medication challenges go far beyond the fundamentals of incorrect dosages or missing meds. Members often experience functional living limitations after a hospital event and may not be able to acquire their prescriptions. They may struggle with socioeconomic limitations or behavioral issues that prevent compliance. Or perhaps they simply do not understand the importance of adhering to their recommended regimens every day.
Using advanced technology to identify these risks and authentic connections with trained clinicians to understand and address any barriers can significantly decrease the likelihood of a medication-related preventable readmission.
Lastly, health plans need to keep the big picture in mind. The TRC metric might technically be a process measure, but its purpose is to prevent avoidable readmissions, reduce costs, and improve member experiences. Health plans need to do everything they can to achieve these outcomes, especially as the relationship between Star Ratings and member experiences draws closer and closer.
Unfortunately, health plans that do not already have an aggressive, proactive strategy to improve their performance on TRC for the current performance year are starting behind the eight ball. TRC verification was required beginning January 1, 2022 and should be occurring daily. All hope is not lost, however. By partnering with highly skilled technology providers, continuing to prioritize patient engagement, and bolstering medication reconciliation processes, health plans can quickly gain ground and score better on the Star Ratings while achieving value-based care’s larger goals.