Published on .
Medication safety has become an urgent priority as Medicare Advantage members increasingly rely on prescription drugs to manage chronic conditions. While many older adults experience polypharmacy—defined as taking 5 or more simultaneous prescriptions—the concern isn’t just the number of drugs taken. It’s the heightened risk that comes when certain classes of medications are combined or misused.
Opioids, benzodiazepines and anticholinergic drugs are particularly high risk. And when used improperly, these drugs can contribute to serious and sometimes fatal adverse events for plan members.
To address these dangers, the Centers for Medicare and Medicaid Services (CMS) has introduced two new Part D Star Measures for 2025: Concurrent Use of Opioids and Benzodiazepines (COB) and Polypharmacy: Use of Multiple Anticholinergic Medications in Older Adults (Poly-ACH). These measures are designed to hold prescribers and health plans accountable for prescribing practices that directly impact member safety—focusing attention not only on the volume of prescriptions, but also on the combinations most likely to cause preventable harm.
“There’s a therapeutic place for all of these medications, but the exponential risk of being on some of these medications together is definitely something that can affect the health of members, as well as the medical spend for the health plan,” explained Levi Sanderson, PharmD, Senior Director of Clinical Solutions at AdhereHealth in a recent webinar exploring how to improve performance on these two high-priority Stars measures.
“In order to perform well on these new measures, health plans need to get proactive about identifying at-risk individuals, connecting with those individuals in a personalized, targeted manner and coordinating care via omnichannel communications to reduce risks, avoid unnecessary spending and improve outcomes for members.”
New measures for monitoring polypharmacy risks
Older adults are particularly vulnerable to medication-related complications, especially when prescribed drugs with sedating or anticholinergic properties. In the clinic, providers may not always have a complete picture of a patient’s medication history, making it easy to miss potentially dangerous combinations. At home, members may not fully understand dosing instructions or may take overlapping prescriptions, further increasing the chance of harm. These scenarios can lead to severe side effects—including confusion, dizziness, falls, hospitalizations and other avoidable medical expenditures—explained Sanderson.
That’s why CMS established the COB and Poly-ACH measures.
The COB measure calculates the percentage of Part D members (18 years or older, so not just the 65+ population), with concurrent use of prescription opioids and benzodiazepines for at least 30 cumulative days during the measurement period.
The Poly-ACH measure focuses only on older adults and calculates the percentage of 65+ members with concurrent use of two or more unique anticholinergic (ACH) medications for at least 30 days during the measurement period.
“It can be a challenge to address polypharmacy with these individuals, especially if they feel that some of these medications are doing them good,” noted Kempton Presley, Chief Executive Officer at AdhereHealth. “And there may be instances where that patient really doesn’t have a good mechanism for discontinuing, or their prescriber may not have a good path or decision support for de-prescribing.”
“That can cause abrasion, but that’s why we’re introducing strategies to assist health plans with shifting prescribing patterns in a positive direction while maintaining good experiences and outcomes for plan members.”
Identifying at-risk plan members as early as possible
The first step is identifying high-risk members long before they fail one of these measures—and before they experience an adverse health event that leads to avoidable medical spend.
“There are several ways to forecast which individuals are likely to end up in the measure or are more likely to fail the measure,” explained Presley. “You could use medical data to highlight people who are having procedures or diagnoses that tend to be associated with pain management prescriptions. You could look at someone’s history with different types of behavioral medications. You could look at claims to see who has unplanned ED events in their recent history. There are a variety of different leading indicators, but you need the right infrastructure to aggregate, visualize and share this data in a way that lets your care teams connect with these members quickly.”
For example, tools from AdhereHealth monitor MA plan members throughout the performance period to identify events that may place individuals in the denominator for the two measures in question, such as a refill request for a short-term opioid or the established use of an ACH medication for incontinence.
“When some of these escalating points start to happen, the platform delivers a clinical direct message into the doctor’s EHR as a nudge to alert the prescriber of potential conflicts and risks with existing medications,” said Sanderson.
Personalizing outreach to avoid escalation of medication risks
It’s important to keep a continuous eye on members with higher risks, especially since prescribers only have a certain number of options to treat complex conditions and provide adequate pain management.
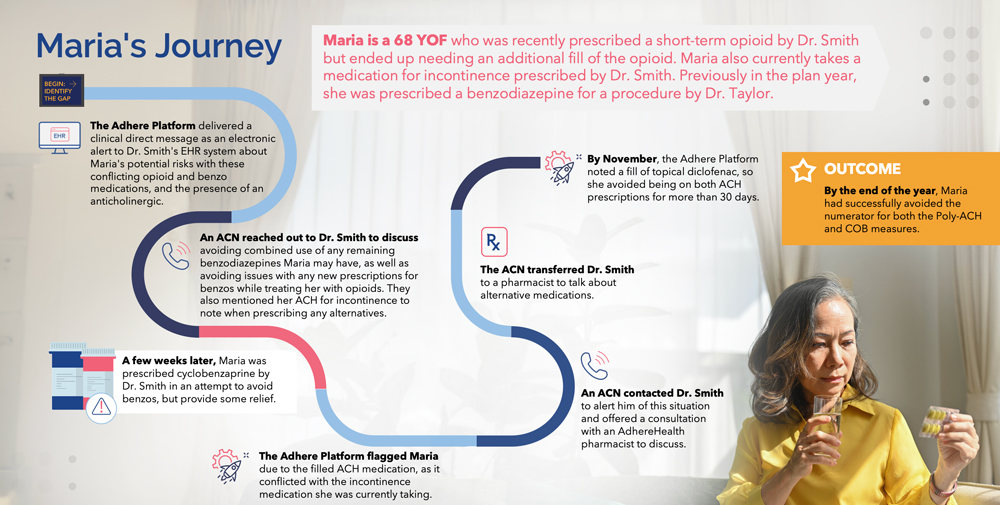
“Let’s think about our patient ‘Maria,’ who’s 68 years old and is taking both a short-term opioid for pain management and an ACH for urinary incontinence, and previously received a short-term benzodiazepine prior to a procedure earlier this year,” said Sanderson. “She’s moving up into higher risk categories with these prescriptions, so we might opt for a more direct telephonic approach from an adherence care navigator (ACN) reaching out to her doctor to reiterate this fact and advise against prescribing benzodiazepines or any additional anticholinergic medications.”
“A few weeks later, Maria was still having pain, so her doctor prescribed some cyclobenzaprine, a muscle relaxer, in an attempt to provide some relief and still avoid benzodiazepines. Unfortunately, cyclobenzaprine is another medication with high anticholinergic properties. It’s such a difficult juggling act for prescribers sometimes and it’s easy to overlook some of these scenarios.”
Once the ACN reached back out to the prescriber to caution against the decision and discuss alternative medications, Maria was able to get a different treatment for her pain and successfully avoid joining the numerator for both the Poly-ACH and COB measures.
“It’s a great example of how a personalized and targeted approach to monitoring and engagement can illuminate those blind spots in a way that fits into the care team’s workflow and gives them the tools and information they need to avoid prescribing something that could be problematic,” said Presley.
Designing omnichannel communications for comprehensive care
These types of direct connections with the care team are essential for pre-empting potentially dangerous prescribing events, said both Sanderson and Presley. But with the ongoing challenges of data interoperability and communication across the care continuum, finding the right touch points to get the message through can be difficult.
“Having multiple ways to communicate is essential for staying proactive on behalf of plan members,” said Presley. “That might be through faxing, emails, phone calls or EHR-integrated messaging—the trick is to have as many of these channels available as possible so there’s the capability to customize interactions to what fits best into the prescriber’s workflow.”
He also suggested that plans should have access to peer-to-peer communicators to work directly with prescribers, not just to deliver administrative information about measure performance but to offer informed counseling and prescribing decision-making support when necessary.
“These are all extremely important and effective ways to get one step ahead of these two new measures,” concluded Sanderson. “With technology to help stay vigilant and strong lines of communication to personalize a comprehensive outreach strategy, plans can really take charge of their performance on the COB and Poly-ACH measures, while meaningfully improving the member experience and keeping them safer and healthier as long as possible.”
Dive into more details about the COB and Poly-ACH measures, including actions plans can take to address them, in our webinar replay: From Risk to Results: A Roadmap for COB and Poly-ACH Measure Improvements.