Published on .
Presenting together with other industry experts at the 2023 RISE Star Ratings Master Class, AdhereHealth Chief Commercial Officer, Glenn Wirick (alongside Kim Shell, Star Ratings expert, and Bert Rico, Director, QI and Clinical Analytics at Baylor, Scott & White Health Plan) dove into the ongoing challenge of “engaging the unengageable” high-risk plan members. The presentation offered real-world strategies for closing gaps and improving member experience as MA plans tackle this “last mile” in their Star Ratings strategy.
Member risk stratification is now a familiar concept to Medicare Advantage plans, but there’s more to effective member prioritization than simply using analytics to establish risk buckets. MA plans also need to have targeted, comprehensive strategies for engaging and managing each of their member cohorts according to their clinical needs and consumer preferences.
This gets harder and harder as plans move up the risk scale to the most complex individuals, who are typically living with multiple comorbidities and significant socioeconomic challenges that may be compounded by behavioral health concerns. As a result, every health plan has a top bracket of high-risk members who are often chronically unengaged in their own care and incur an outsized proportion of spending. Across the Medicare continuum, the costliest 5% of individuals are responsible for approximately half of all spending, while experiencing more challenges with care coordination and managing multiple prescriptions.
These members represent the “last mile” of success for MA plans; they are usually the group most plans struggle to reach and the cohort they are often least able to successfully engage in activities required by CMS to meet 4.0+ Stars performance thresholds. This is particularly critical as the Star Ratings system evolves to put an even brighter spotlight on health equity, care coordination and medication adherence.
From the new Health Equity Index (HEI) and proposed Hold Harmless adjustment, to anticipated changes to the medication therapy management (MTM) program and triple-weighted medication adherence measures that can directly impact access to incentive opportunities, MA plans have a very clear and immediate motivation to establish adherence strategies with their chronically unengaged, highest-risk members.
To effectively and efficiently engage these members while achieving better Stars results, MA plans will need predictive analytics and a personalized approach from clinical teams with the bandwidth to assist with strategically managing chronic conditions and non-clinical barriers.
Who are the chronically unengaged?
Chronically unengaged members have varying levels of unique needs. They may have had few or no healthcare visits in the past 12 to 24 months, despite having potentially problematic diagnoses on record. They may be experiencing significant gaps in care or misaligned goals with their clinical teams. They could be unreachable by traditional contact methods, they may intentionally avoid calls from the health plan, or they might simply be unaware that they should be in touch with their providers and health plan.
But more importantly, unengaged individuals may have a number of different socioeconomic reasons for experiencing these indicators. The social determinants of health (SDOH), including food and housing insecurity, transportation barriers, low health literacy and social isolation, tend to have a significant impact on a person’s ability to manage their health. Behavioral and mental health issues, such as depression and anxiety, also play a role in the degree of engagement among health plan members.
It isn’t enough to just identify a person who meets a plan’s specific criteria for being unengaged. The plan must also understand drivers of non-engagement and have a multimodal approach to driving engagement in this most difficult member cohort.
Successfully reaching chronically unengaged members
Plans shouldn’t rely on a “one-size-fits-all” approach to improve Star Ratings throughout the entire member population. In fact, the most vulnerable members require different approaches that prioritize SDOH barrier resolution as a foundational strategy to address members’ nonadherence with Part D and Part C measure criteria.
It starts with harnessing the power of a technology platform that identifies members with adherence and HEDIS gaps, but also takes into account SDOH factors and dispositions from previous interventions. Using this combination of data, the platform then automatically predicts the “next best action” for outreach to the member at the right time, with the right type of support.
From there, driving engagement with the chronically unengaged takes a multi-pronged approach supported by the right technology platform. Being able to report on and update incorrect member contact numbers is “table stakes,” required for initiating the engagement process. Additionally, to employ all opportunities for the clinician to make contact with a hard-to-reach member, a technology solution should serve up rotating phone numbers, including those that display local presence, as well as toll-free numbers, and alter the time of day and time of month for calling. Why time of month? Because many financially challenged members have prepaid phones that run out of minutes toward the end of the month. Therefore, the platform should automatically tee up calls for the first week of the month, when connection was not made earlier in the month.
The technology platform should also give full visibility to all providers supporting a member, and automatically cue outbound clinician-to-clinician interaction with providers to drive engagement with uncontacted members. This method can be employed for members who haven’t answered phone calls, those with disconnected numbers, and even members on the health plan’s “do no call” list. It’s also critical to utilize multilingual clinicians to connect with members in their primary language, and with a real human voice (not IVR, which can lead to automatic hangups).
Another helpful technique (if the clinician isn’t able to reach the member) is to leave a human (not IVR) voicemail that emphasizes, in the member’s primary language, that support and help are being offered, rather than actions being requested. It’s often the case that, over and over, members appreciate the concept of “help” and are more prone to engage through the offer of help.
Systemically identifying barriers and addressing non-clinical concerns
It’s not enough to simply acknowledge a member’s nonadherence, but instead get a thorough understanding of what’s behind it.
With the growing recognition that SDOH barriers greatly contribute to healthcare spending and health outcomes, federal, state and local datasets are available to support more advanced population health analytics. Integrating these types of datasets into clinical analytics models can give MA plans much deeper insight into members and their needs.
MA plans should seek out platforms that deeply integrate publicly available SDOH data, such as the Social Vulnerability Index (SVI), provided by the CDC, with clinical and administrative analytics to create highly detailed, easy-to-interpret dashboards and visualizations. SVI data surfaced to the outreach clinician provides key information into the challenges faced by the member. This type of data-driven technology can provide tailored insights that help plans understand and stratify the level of risk faced by plan members in need of outreach.
Health plans can also work the problem from the other side by actively collecting information from members during provider interactions or plan outreach engagements. There are several low-code tools available to aggregate this data in a structured manner so it can be integrated into broader analytics efforts, such as MS Forms or Google AppSheet.
MA plans can then correlate socioeconomic vulnerabilities with their chronically unengaged cohorts, map their existing initiatives against the most pressing needs in their member populations, and develop new interventions that are targeted to these specific areas and aligned with the relevant Star Ratings performance metrics.
Personalizing care to build trusted, lasting relationships
Another valuable technique is motivational interviewing, which helps the clinician build a meaningful relationship with the member based on trust and mutual respect.
Once uncovered, SDOH barriers can be resolved through real-time education about plan benefits or referrals to community resources for support. This SDOH-first approach improves adherence by removing underlying barriers impeding it.
Plans should also consider adapting to member communication preferences. For example, plans need to know if their high-risk members don’t use email, don’t have a stable home address to receive mailings, don’t have enough minutes on their pre-paid cell phone each month, prefer a language other than English, or simply can’t navigate complicated phone trees before they reach a person. Gathering details like these about communication preferences—and having enough options to meet the member’s needs—is crucial for reaching the unreachable and maintaining contact over time.
All information about the member should be recorded in a shared tool for closed-loop communication with the health plan and pertinent follow-up with the member—building on year-long, longitudinal adherence with behaviors that drive both improved health outcomes and Star Ratings performance.
Patient success story

One example of the positive outcomes members can realize through SDOH barrier resolution for improved medication adherence is 65-year-old Mr. Brooks (name changed to protect privacy), a member on a Medicare Advantage plan that partners with AdhereHealth. This member lives with diabetes, hypertension, glaucoma and severe vision loss, as well as inconsistent access to healthy food and reliable transportation.
When the Adhere Platform rules engine identified Mr. Brooks for outreach regarding an adherence risk with his hypertension medication and an overdue diabetic retinal exam, an AdhereHealth outreach clinician contacted him and discovered he lacked access to transportation, plus was also faced with food insecurity. The clinician worked with Mr. Brooks to connect him with food assistance, enroll him in prescription delivery, schedule a diabetic retinal exam, and coordinate transportation provided by his health plan so he could attend his appointment.
With these interventions, Mr. Brooks was able to move back into medication adherence through access to his prescription, and complete his diabetic retinal exam, which also helped his health plan check off the relevant measure.
Client case study
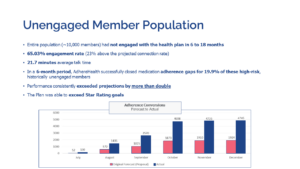
The positive results of data-driven, personalized engagements also quickly stack up at the health plan level. When a national MA plan partnered with AdhereHealth to address the needs of its chronically unengaged members, they identified a group of approximately 10,000 people who had not engaged with the health plan in 6 to 18 months.
AdhereHealth’s experienced telepharmacy outreach team leveraged a combination of advanced analytics and personalized communications to reach more than 65% of these individuals—23% above the projected connection rate.
By spending an average of nearly 22 minutes per call with each member diving into their clinical and non-clinical challenges, the team was able to achieve remarkable results for the members and their plan.
In a 6-month period, AdhereHealth was able to successfully close medication adherence gaps for 19.9% of these historically unengaged members, exceeding projections by more than double and assisting the plan with surpassing their Star Ratings goals.
Tackling the “last mile” of the chronically unengaged population is a challenge for Medicare Advantage plans, but it’s one that is well worth the effort. With a combination of analytics and personalized relationship-building, members living with the most complex conditions can achieve better health and outcomes, while health plans can improve their performance on the Star Ratings and realize the associated benefits.
To learn more about how AdhereHealth approaches personalized engagement for high-risk members, contact us today to schedule a consultation.
 Authored by:
Authored by:
Glenn Wirick
AdhereHealth Chief Commercial Officer
