Published on .
Healthcare plans face an extremely challenging environment when faced with the daunting task of boosting health and well-being in their member populations. The attempt to provide affordable and high-quality care is set against the backdrop of rising chronic disease and a rapidly aging population. For example, the number of Americans with diabetes is projected to triple by 2050, and those with heart disease, heart failure and stroke is expected to increase by close to a third by 2060.
Within this already burdened healthcare landscape, the Medicare Advantage (MA) community currently sits at a crossroads of conflicting forces. On one hand, the rise of consumerism and increasing choices for beneficiaries around MA coverage makes it vital for plans to offer as many attractive, high-quality services as possible to retain or grow membership. On the other hand, regulatory actions like the Inflation Reduction Act and the anticipated changes to Medication Therapy Management (MTM) program criteria are forcing MA plans to think of creative ways to trim spending and compensate for the resulting financial squeeze.
With the right technology and a coordinated clinical approach to outreach and engagement of members, health plans can improve population health outcomes to reduce medical spending, as well as reach their government-sponsored performance program goals.
For MA plans, the need to maintain 4.0+ Star Ratings and earn quarterly bonus payments (QBPs) drives the need for successful plan performance. Clinician outreach and engagement efforts, supported by data-driven technology, is a must to drive member adherence with medications and treatments, thus helping the plan score well on Star Ratings measures. And when faced with the expected influx of changes to MTM measure parameters, the steps plans take to guide members towards adherence will also be critical to improve health outcomes for savings on future medical costs, thus helping fund the MTM program expansion.
As a key member of the clinical team, pharmacists play a vital role in these missions. And their efforts are made even stronger when backed by a robust technology platform that boosts their clinical insights with the power of data.
 Expanding the role of the pharmacist
Expanding the role of the pharmacist
Pharmacists draw from their extensive training in medication dispensing and drug interactions to help ensure a patient is taking their prescriptions safely and appropriately. Beyond work in a clinical setting, digital pharmacy, or “telepharmacy,” has become a more convenient means to reach a greater number of patients. This is especially valuable in rural and urban areas across the country where pharmacy deserts are common—leaving individuals within these communities at a disadvantage when it comes time to fill prescriptions and stick to medication regimens.
Through phone contact with patients, telepharmacy allows pharmacists to connect with a greater volume of patients, performing tasks that directly contribute to patient health and well-being. This could include conducting comprehensive medication reviews (CMRs) as part of the MTM program, or adherence coaching that helps ensure patients to resolve drug therapy problems (DTPs)—drug-related events that can interfere with a patient’s ability to follow optimal treatment therapies.
Identifying and targeting DTPs is a surefire way to improve the health outcomes of members and, in turn, reduce medical spending. As part of an MTM program, MA plans are required to provide CMRs as a key program component—which are invaluable to helps plans uncover and resolve DTPs.
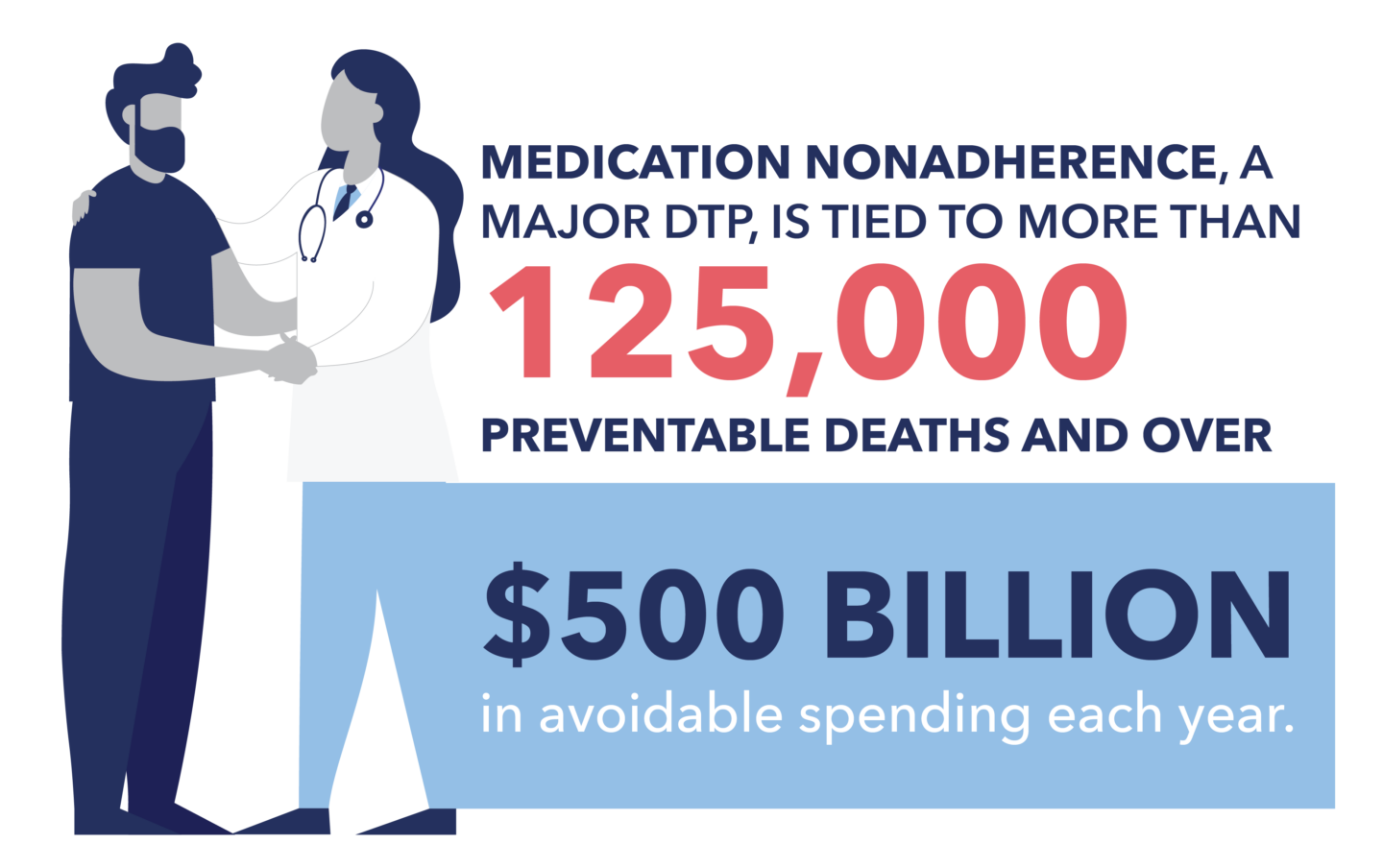 Medication nonadherence, a major DTP, is tied to more than 125,000 preventable deaths and over $500 billion in avoidable spending each year, making it a prime target for health plans that want to get upstream of expensive hospital and emergency room services while providing proactive, comprehensive care to their members. When plans can maximize identification of DTPs, they can also maximize their resolution, leading to improved adherence, plus avoidance of other health and safety issues related to suboptimal medication use.
Medication nonadherence, a major DTP, is tied to more than 125,000 preventable deaths and over $500 billion in avoidable spending each year, making it a prime target for health plans that want to get upstream of expensive hospital and emergency room services while providing proactive, comprehensive care to their members. When plans can maximize identification of DTPs, they can also maximize their resolution, leading to improved adherence, plus avoidance of other health and safety issues related to suboptimal medication use.
The dedicated service of clinical pharmacists is a key role, especially when services are conveniently available to plan members through telepharmacy.
The value of telepharmacy to MA plans
Within an MA plan, a pharmacist is tasked with performing the required CMR as part of the MTM measure—and the better and more complete the data they have to work with, the more efficient and holistic the CMR will be.
A robust data source supports pharmacists in providing the broadest view of all the medications the member may be taking, helping them uncover and resolve the most possible DTPs. This paves the way for improved health outcomes, but also cost savings, on the way to scoring a 4.0+ Star Rating on the MTM measure.
The right technology platform can provide additional details that both support pharmacist interventions and drive additional cost savings. A platform that utilizes medical claims data alongside pharmacy claims data can help surface critical details for pharmacists, such as ICD-10 diagnosis codes and J-codes (which when compared can help indicate a treatment gap if a prescription is absent). NDC codes are an additional detail that can guide a pharmacist to recommend transition to a lower-cost medically equivalent drug or administration site, leading to bonus savings for the patient and plan.
Telepharmacy to improve population health through medication optimization
Beyond the MTM measure, telepharmacy provides health plans with the expertise to drive medication optimization—an endeavor that functions best when supported by the right technology. It all starts with the identification of DTPs, and by maximizing the resolution and closure of DTP gaps, plans can drive improved health outcomes for significant medical cost savings through avoidance of future health issues.
 A technology platform that features predictive analytics and leverages both medical and pharmacy claims offer the advantage of uncovering the greatest number of DTPs for targeted resolution. The platform should be able to identify and group members by provider, information that can then be supplied to the provider as an alert for necessary outreach and resolution.
A technology platform that features predictive analytics and leverages both medical and pharmacy claims offer the advantage of uncovering the greatest number of DTPs for targeted resolution. The platform should be able to identify and group members by provider, information that can then be supplied to the provider as an alert for necessary outreach and resolution.
In addition, the platform should identify and prioritize members for pharmacist outreach to provide clinical intervention and guidance that allows for DTP resolution. A key aspect of this is motivational interviewing—allowing the pharmacist to connect with the patient, understand their unique needs and barriers, and provide education and guidance on medication administration, potential side effects, etc.
By helping members avoid potential non-optimal medication utilization, pharmacists are a critical ingredient in DTP resolution, improved health outcomes and patient experiences, and higher medical cost reduction.
Supporting telepharmacy with technology to achieve value-based performance and savings
Taking a coordinated, strategic approach to medication adherence through telepharmacy can bring significant rewards to health plans, including higher performance on the Star Ratings scale for MA plans, or reduced downstream costs related to preventable hospital and ED use across the board.
Plans should look for technology tools that will support both the current and future needs of the member population, especially as the burdens of chronic diseases continue to increase across all segments of society. Telepharmacy platforms should be able to integrate multisource data to generate complete portraits of individuals and populations, as well as be able to suggest the “next best action” for pharmacy users to help build strong, non-abrasive relationships with higher-risk members.
By leveraging tech-enabled telepharmacy to connect with members, expand access to prescription drugs, and resolve medication adherence issues, health plans will be positioned to remain competitive in the marketplace, maximize their Stars potential or performance on government-sponsored performance programs, all of which can lead to long-term financial sustainability and clinical success.
In need of clinical services or telepharmacy engagement supported by robust, data-driven technology? Contact AdhereHealth to discover how our tech-enabled services help your plan identify and resolve DTPs, for medical cost reduction and top-level performance on the MTM measure.
 Authored by:
Authored by:
Glenn Wirick
AdhereHealth Chief Commercial Officer
