Published on .
Medicare Advantage Special Needs Plans (SNPs) play a critical role in providing tailored healthcare solutions to some of the most vulnerable populations—older adults with specific healthcare needs. These plans are designed to address unique challenges faced by elderly members, many of whom have chronic health conditions, financial limitations and a higher risk of medication nonadherence.
The combination of these factors often produces challenges with establishing and maintaining engagement, particularly among members who may be unable or unwilling to consistently interact with their healthcare providers and health plans. Often, these members are deemed “unengageable” by the plan (e.g., difficult to connect with in the first place, or difficult to engage with once successfully reached).
An “unengageable” status typically results in poorer member health, either due to a yet-unidentified health need, or due to gaps in care and medication nonadherence. These situations can result in reduced performance on the Star Ratings system for SNPs, which translates to higher costs, ebbing enrollment rates and limited access to financial incentives, such as the Quality Bonus Program (QBP), that are crucial for sustainability in a highly competitive marketplace.
Through partnership with the right technology partner, allowing for robust healthcare data analytics that empower the work of telepharmacy staff, SNPs can take action yet in 2024 to complete CMS Star Ratings COA measure assessments and drive toward 4.0+ Stars. They can also use this outreach opportunity to uncover and resolve care gaps and drug therapy problems (DTPs) that improve future health outcomes and reduce associated medical spending.
CMS continues to challenge MA plans
MA plans are under constant pressure to maintain the health of their members, particularly those in SNPs who often have more complex healthcare needs. This involves engaging members in medication adherence, regular health screenings and other preventive measures that contribute to their overall well-being.
Meeting the rigorous requirements set by CMS is no small feat. MA plans, including SNPs, must continuously strive to improve their performance to retain high Star Ratings and remain competitive in an ever-evolving healthcare landscape.
SNPs face additional hurdles due to the unique needs of their member populations. This cohort is among some of the most vulnerable and medically complex in the country, including those experiencing significant health concerns and major barriers related to social determinants of health (SDOH).
According to recent statistics, the number of older adults in the U.S. with two or more chronic conditions is expected to increase from 7.8 million (over half the population of adults age 50 and older) to 15 million (almost 70% the projected adult population in 2050). Adding to this, many SNP members—simply by definition—suffer from chronic health conditions, such as diabetes, heart disease and COPD, which require ongoing management and coordination of care. These chronic conditions often lead to complex medication regimens, which can increase the risk of nonadherence—a significant challenge in maintaining the health of SNP members.
The evolving requirements of COA
The COA measures are essential quality performance metrics for SNPs and include a comprehensive pain assessment and an annual medication review. These assessments are crucial in ensuring that older adults receive the appropriate care to manage their health conditions and maintain their quality of life, plus are required by CMS for every SNP to complete for every member aged 66 years and older.
Starting in MY 2025, NCQA has retired the pain assessment indicator of the COA measure, as it did not effectively differentiate between acute and chronic pain. The functional status assessment indicator, a display measure in MY 2024, is expected to be brought back for MY 2025. This shift reflects the growing recognition of the importance of functional assessments in identifying early signs of decline in older adults, which can help in planning interventions that preserve their independence and well-being.
Completing the COA assessments not only ensures compliance with CMS requirements but also positively impacts a plan’s Star Ratings and ability to maintain a competitive position in the managed care marketplace.
The value of a focus on COA measure completion—plus additional advantages
The advantages of COA measure completion are both direct and indirect, and serve to benefit the performance and longevity of a SNP.
On the surface, COA measures form the basis for creating an advanced care plan, a critical component of a SNP’s Model of Care (MOC). The MOC is a comprehensive plan designed to identify and address the unique needs of each enrollee, ensuring high-quality care management and coordination.
The National Committee for Quality Assurance (NCQA) evaluates the MOC as part of the SNP approval process, with plans required to score above 70% to receive final approval to operate for up to three years. By successfully completing COA measures, SNPs can demonstrate their commitment to high-quality care, ensure completion of their MOC and therefore boost their score with the NCQA.
Beyond these more obvious benefits of COA completion are other more indirect advantages, which can be realized through partnership with a robust healthcare data analytics solution. Access to a comprehensive data set provides outreach pharmacists the ability to surface critical data and details about individual members, which can maximize interactions during COA assessment completion.
Many SNP members may not otherwise qualify for an in-depth pharmacist review (such as that available through MTM, for example) and when that interaction is boosted by access to a robust data platform, care gaps and DTPs can be surfaced either through clinical data or conversation—providing an opportunity for the pharmacist to discuss and resolve healthcare issues that may not have otherwise been uncovered (for example, a lapsed medication fill, drug/drug interactions or a diagnosis without a related prescription). This engagement provides a chance for the plan to improve member health outcomes and prevent medical spending associated with worsened health conditions, had they not been resolved.
Best practices for engaging the SNP population
To connect with difficult-to-engage plan members, SNPs need to deploy a combination of leading-edge technology and person-centered outreach. They should look for partners or other capabilities that can perform the following tasks:
Proven multi-modal outreach and engagement techniques
Making that initial member contact can be made easier with a dedicated partner offering proven multi-modal outreach capabilities, such as a combination of analog and digital techniques, to establish connection with the hardest-to-reach members. Materials should be provided in the member’s language of choice and all points of contact should be clear about their purpose and goals, including person-to-person conversations. Then, plans can successfully accomplish COA assessments and check other Star Ratings measures off the list.
When developing outreach programs, plans must account for the subtle complexities of communicating with individuals facing social determinants of health (SDOH) challenges. For instance, understanding when lower-income members are likely to have available phone minutes or identifying the optimal time to reach those working night shifts or providing constant care for a loved one can make a significant difference. Approaching these situations with sensitivity and respect will allow plans to build stronger connections with these harder-to-reach members, establishing a solid foundation for more meaningful relationships.
Enhanced data insights to empower clinical intervention
Data analytics are essential for gaining a deeper understanding of how and when DTPs occur. By leveraging the right technology platform to integrate and analyze both medical and pharmacy claims data, MA plans can identify and address a greater number of DTPs. This approach may also reveal additional cost-saving opportunities, such as identifying ICD-10 codes without corresponding National Drug Code (NDC) pharmacy claims or transitioning to more affordable specialty drugs.
With more comprehensive data on member utilization and prescriptions, pharmacists can perform more effective comprehensive medication reviews (CMRs) and resolve potential issues before they escalate into costly crises. The technology tools used should feature intuitive dashboards and streamlined workflows that enable clinical outreach staff to quickly identify concerns and engage with members with minimal disruption.
Identification and resolution of specific barriers to improve experiences and outcomes
During the member engagement process, outreach staff can also strive to identify specific issues that may be solved with clinical interventions, unused health plan benefits or community-based referrals for SDOH concerns. This includes identifying DTPs, socioeconomic barriers to medication access, and functional limitations that could interfere with appropriate medication adherence—helping improve the health outcomes of these members beyond just COA assessments.
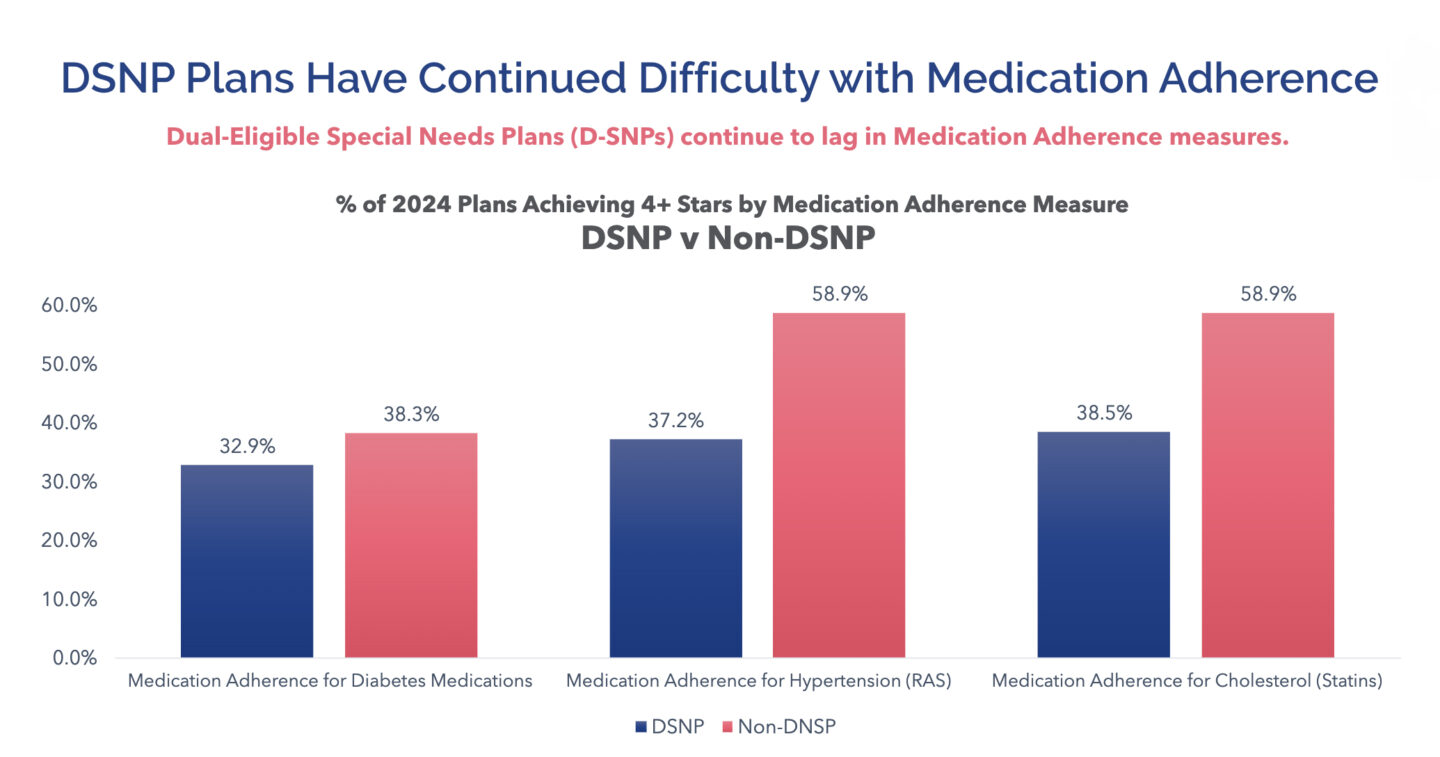
Since medication adherence has such a profound impact on overall Stars performance, prioritizing these issues during member engagements can produce outsized returns for the plan and the individual member.
SNPs have strong incentives to reexamine their highest-risk, hardest-to-engage members and make a concerted effort to maximize outreach efforts with these cohorts. Financial sustainability and continued competitiveness are on the line for those who do not successfully meet the COA thresholds in combination with medication adherence measures and other foundational Stars performance metrics.
Take action now to engage “unengageable” members for COA completion and additional cost reduction
There is still time in MY 2024 to ensure that your SNP completes specific Star Ratings measures and meets CMS requirements. Don’t wait—take action now to secure your plan’s future and continue to provide the best care possible for your older adult members. Align with a data-driven healthcare technology partner who can help you navigate successful Star Ratings performance, as well as the COA process, to achieve the best outcomes for your plan and its members.
To learn more about the healthcare analytics-driven SaaS and tech-enabled telepharmacy solutions available through partnership with AdhereHealth, contact us today!

AdhereHealth Senior Director of Clinical Solutions
