Published on .
As Medicare Advantage plans grapple with rising cut points from the 2025 Star Ratings and strategize for performance improvements, one thing is clear: effectively engaging and motivating members to complete measure-specific behaviors is critical to a successful Stars strategy.

Dr. Chandra Osborn has recently joined the AdhereHealth Executive Management team as its Chief Behavioral Officer, bringing over 25 years of experience as a behavioral scientist and business leader. Her expertise spans patient engagement, medication adherence, digital personalization and behavior change strategies to drive both health and business outcomes. In her role, Dr. Osborn will help further integrate behavioral insights into client interactions, and business and product development—enhancing AdhereHealth solutions, credibility and market impact.
In other words: she’s the go-to expert for health plans struggling to improve Star Ratings performance, especially with members that are hard to reach and difficult to engage.
We sat down with Dr. Osborn for insight into her background, what has led her to AdhereHealth and how her influence will be helping us shape the effectiveness of our adherence solutions:
1. Can you share a little bit about your journey? How have your previous experiences shaped your approach to behavioral science and improving health outcomes?
I’ve spent nearly 25 years designing digital health solutions and applying behavioral science to improve health outcomes. My background as an NIH-funded investigator, executive roles in digital therapeutics, and leadership in AI-powered behavior change companies have given me a deep understanding of how to blend science with technology to engage consumers, promote healthy actions and improve health outcomes effectively. These experiences shape my data-driven approach to creating scalable interventions that impact patient engagement and medication adherence to improve health and health equity.
2. Behavioral science and digital health solutions are increasingly intertwined. How do you envision integrating these fields to improve medication adherence and overall member engagement?
Behavioral science helps us understand and influence how individuals think, decide and behave, while digital health solutions provide the platform to deliver personalized interventions at scale. By combining both, we can create more engaging experiences that meet members where they are to overcome their barriers to medication adherence—leveraging AI, tailored messaging and data analytics to influence behavior in real-time. This integration is essential for improving medication adherence and sustaining long-term engagement, particularly in hard-to-reach populations.
3. What are some of the most effective strategies for driving behavior change in Medicare Advantage members? Are there specific examples where you’ve seen these strategies succeed?
Overcoming member barriers with personalized messaging has proven effective. At AdhereHealth, we use data-driven insights to identify members who are nonadherent, target outreach using our multimodal capabilities and provide tailored interventions, improving adherence and outcomes.
One success story involves a member who we identified as having a gap in her blood pressure medication refills. When we connected with her, we determined she was the sole caregiver for her husband, who had dementia. She was so overwhelmed each day with his care that she was forgetting to take her own medication. She was isolated and didn’t have anyone to talk to, or any support for herself. Our AdhereHealth Care Navigator walked through this member’s day with her to understand what she was facing and provided behavioral triggers for how to stay on track with her medications, plus set her up with mail order to help with her refills. They also connected her with local caregiver support groups for people in similar situations that she could talk to. This resulted in a measurable increase in the member’s adherence with her medication.
4. Medicare Advantage members can be hard to reach and engage. What are the biggest challenges in promoting behavior change among these members and how would you overcome them?
Challenges include socioeconomic barriers, limited health literacy, distrust in the system and several knowledge, motivations, skills and problem-solving barriers. Overcoming these requires empathy, clear communication and meeting members where they are—whether through multi-channel outreach or tailored messaging. Leveraging trusted relationships, like those built by AdhereHealth’s highly skilled and trained Care Navigators, and incorporating behavioral science, can further enhance engagement and trust.
5. What emerging trends or technologies do you believe will play a pivotal role in advancing behavior change in healthcare? How can health plans leverage these trends to stay ahead?
Emerging trends like artificial intelligence, telehealth and wearable technology are pivotal in advancing behavior change in healthcare. AI can personalize interventions and predict adherence issues, while telehealth offers convenient access to care and support. Wearable devices can provide real-time health data, encouraging proactive health management. Health plans can leverage these trends by integrating them into their member engagement strategies, ensuring that interventions are data-driven and tailored to individual needs, thereby enhancing overall member experience and outcomes.
6. Looking ahead, how do you see the role of behavioral science evolving in the next five to ten years, particularly in the context of Medicare Advantage and Star Ratings?
Behavioral science will play a growing role in personalizing care and driving member satisfaction, both key components of Star Ratings. As AI and machine learning become more sophisticated, we’ll see greater precision in predicting behaviors and tailoring interventions, helping health plans achieve higher ratings by proactively addressing gaps in care, improving outcomes and enhancing the member experience.
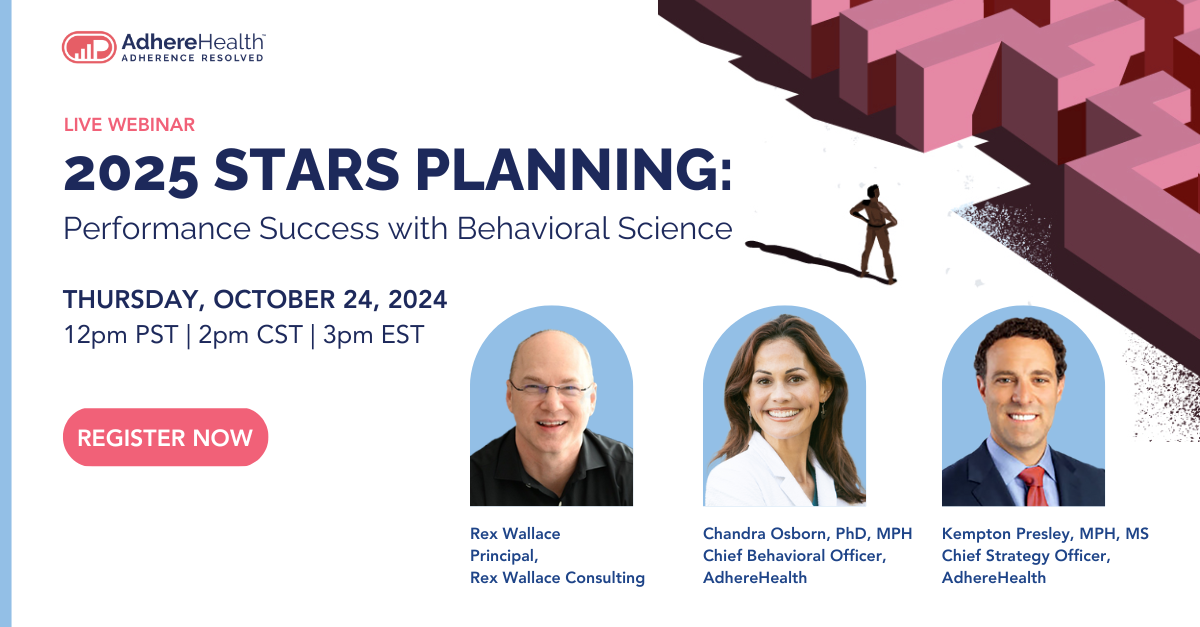
Gain insight into tackling your plan’s Star Ratings performance with a focus on behavioral science techniques when you join our upcoming webinar: 2025 Stars Planning: Performance Success with Behavioral Science on October 24, 2024. Register today!