Published on .
It’s time to make a wish, because the Stars are falling. The recent 2025 release from the Medicare Advantage (MA) Star Ratings program reflects the toughest quality bonus program (QBP) year ever for MA plans, with the average Star score dropping precipitously from 4.07 to just 3.92. It’s the first time since 2015 that the average sank below 4.0, even during the pandemic years when health plans struggled with Stars performance and scores were bolstered by CMS safeguards.
The drop in the 2025 Star Ratings was largely driven by regulatory and legal changes to the program framework. This will have a major impact on health plans and their ability to access incentive dollars from the QBP. But it will also have a significant effect on members, including their healthcare spending, benefits coverage and experiences with their health plans. With dramatically fewer 4-Star and 5-Star plans for the upcoming 2025 plan year, the percentage of members covered by top-performing options has also shrunk dramatically, from 76% to just 62% of members. This means 14% of the market will see higher premiums, higher cost sharing and less benefits in 2025 than they had before.
This should be setting off warning bells for the many plans that experienced notable score reductions. Member turnover is likely to increase, as consumers seek more value for their money, which could disrupt financial sustainability and further reduce performance on key member experience measures, such as CAHPS, that have propped up historical Stars scores.
There’s no question that it’s a grim environment for MA plans, and future regulatory adjustments to the ecosystem are likely to make it even tougher. However, MA plans are far from helpless against sinking Star Ratings. Plans need an innovative approach to successful performance through not only influencing member behavior but also increasing members’ access to care and how they understand the healthcare information they’re being presented. Through an approach based on behavioral science, plans can check off all these boxes, helping to maximize their limited resources in a Medicare landscape where the targets are only getting harder to hit.
2025 Stars planning: performance success with behavioral science
In a recent webinar from AdhereHealth, Chief Strategy Officer, Kempton Presley, MPH, MS, and Chief Behavioral Officer, Chandra Osborn, PhD, MPH, were joined by Rex Wallace, Principal at Rex Wallace Consulting to discuss the current CMS Star Ratings climate and share strategies for navigating the Medicare market’s upcoming challenges.
Their recommendations center on taking a new approach to identifying areas for improvement and fostering organic, sustained member engagement by employing tips and tricks rooted in behavioral science.
Need to improve your Star Ratings? Watch our full webinar replay for insight!
Understanding the Stars framework through the lens of behavioral science
Overall, the Star Ratings system exists to improve the quality of healthcare, thereby improving health outcomes. To do so, the scoring rubric focuses on ensuring that plans and providers are accountable for members’ health and satisfaction, and that plans perform the right activities to assist members with accessing care and making informed decisions about their health.
As such, MA plans can sort Star Ratings measures into four major domains:
- Measures driven by member behaviors (e.g., adherence to prescribed medications)
- Measures driven by provider behaviors (e.g., routinely delivering cancer screenings)
- Measures to gauge member experiences with the health plans (e.g., availability of foreign language interpreters in the call center)
- Measures to gauge member experiences with their care providers (e.g., ease of making a timely appointment)
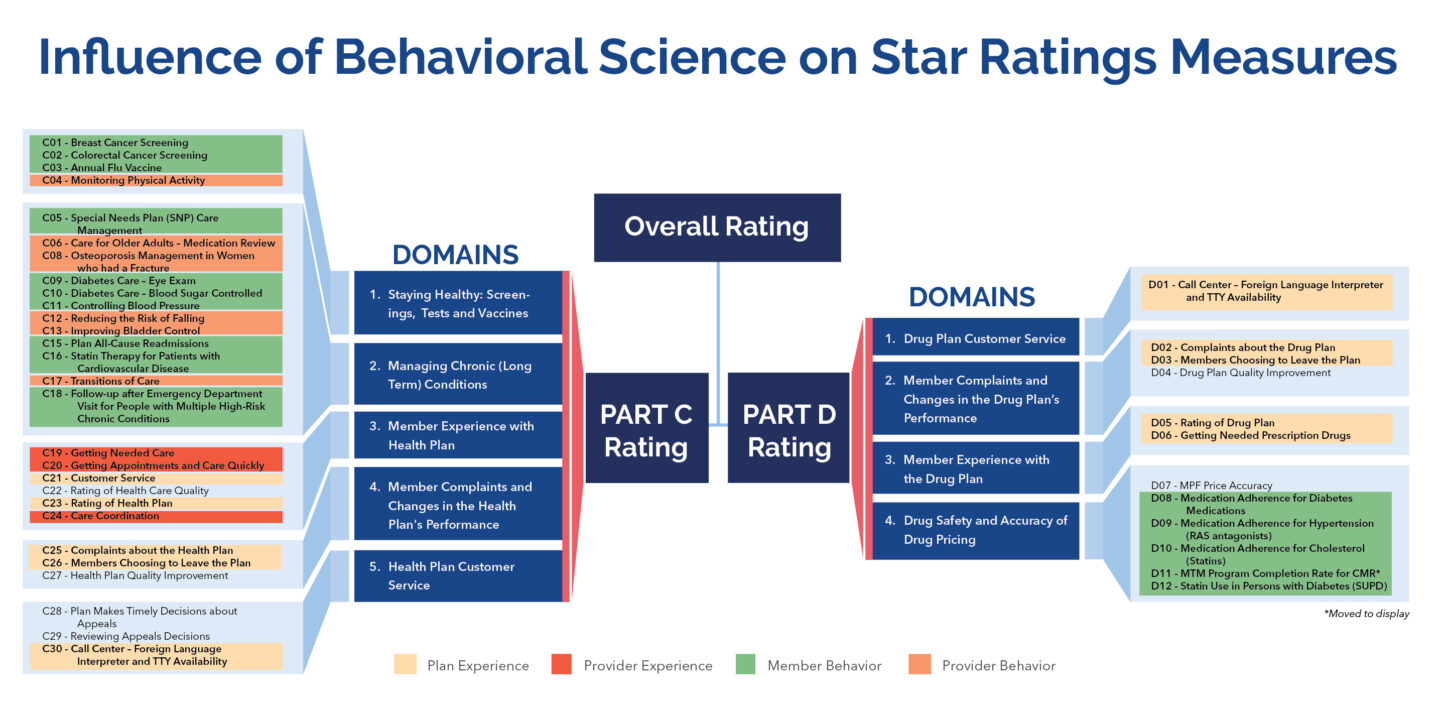
This system of organization is useful because it highlights the relationships between action and reaction, giving plans a better sense of which party to target when attempting to influence an outcome. That’s the core of a behavioral science approach to enacting change—to act as a sort of “decoder ring” to help inform the Star Rating strategy that plans employ for successful performance.
Behavioral scientists deeply understand how and why people behave the way they do and can use that information to behaviorally design programs and experiences that increase a desired behavior or response. For health plans, this means using the principles of behavioral science to design programs and experiences that catalyze desired member and provider behaviors, and members’ survey responses, respectively, to earn higher marks on the Stars measures tied to higher overall scores and more opportunities to access incentives.
A foundational solution for a well-rounded Stars strategy
The influence and ultimate importance of a behavioral science–based approach can be far-reaching. Given the limited resources plans are often faced with—for example, there are only 12 months in a calendar year to enact positive behavior change, and only so many members of the clinical team to support members’ needs—it’s important for plans to be strategic with how to dole out resources and maximize the impact of their efforts. A Stars strategy rooted in behavioral science helps plans not only improve successful Stars performance, but extend that success throughout the Stars framework. As a proven means of understanding and driving members’ and providers’ behaviors (including members’ survey responses), behavioral science gives MA plans an innovative edge in an environment that is becoming increasingly difficult to navigate and conquer.
By incorporating evidence-based tactics through partnership with a trusted behavioral science partner, plans can leverage guidance that informs when and where to assign resources in ways that will deliver the biggest yield throughout the full Stars portfolio of measures. This is not just convenient, but rather imperative to continue successful Star Ratings performance, earn coveted QBP incentives and remain competitive in the Medicare marketplace.
AdhereHealth provides evidence-based Star Ratings strategies that help MA plans improve member engagement, health outcomes and measure performance. Want to learn more? Contact us to schedule a consultation.