Published on .
Medication adherence, like life itself, is a journey—not a destination. And for Medicare Advantage (MA) plans, it’s essential to support members through their unique and evolving adherence journeys. This is necessary throughout the current calendar year and with each passing year, as members re-enroll and their needs change.
A long-term, personalized strategy is crucial to helping members successfully initiate and maintain adherence improvements. This is vital for achieving 80% of the proportion of days covered (PDC) for a member population, which directly impacts performance on triple-weighted Star Ratings adherence measures.
The challenge of medication adherence
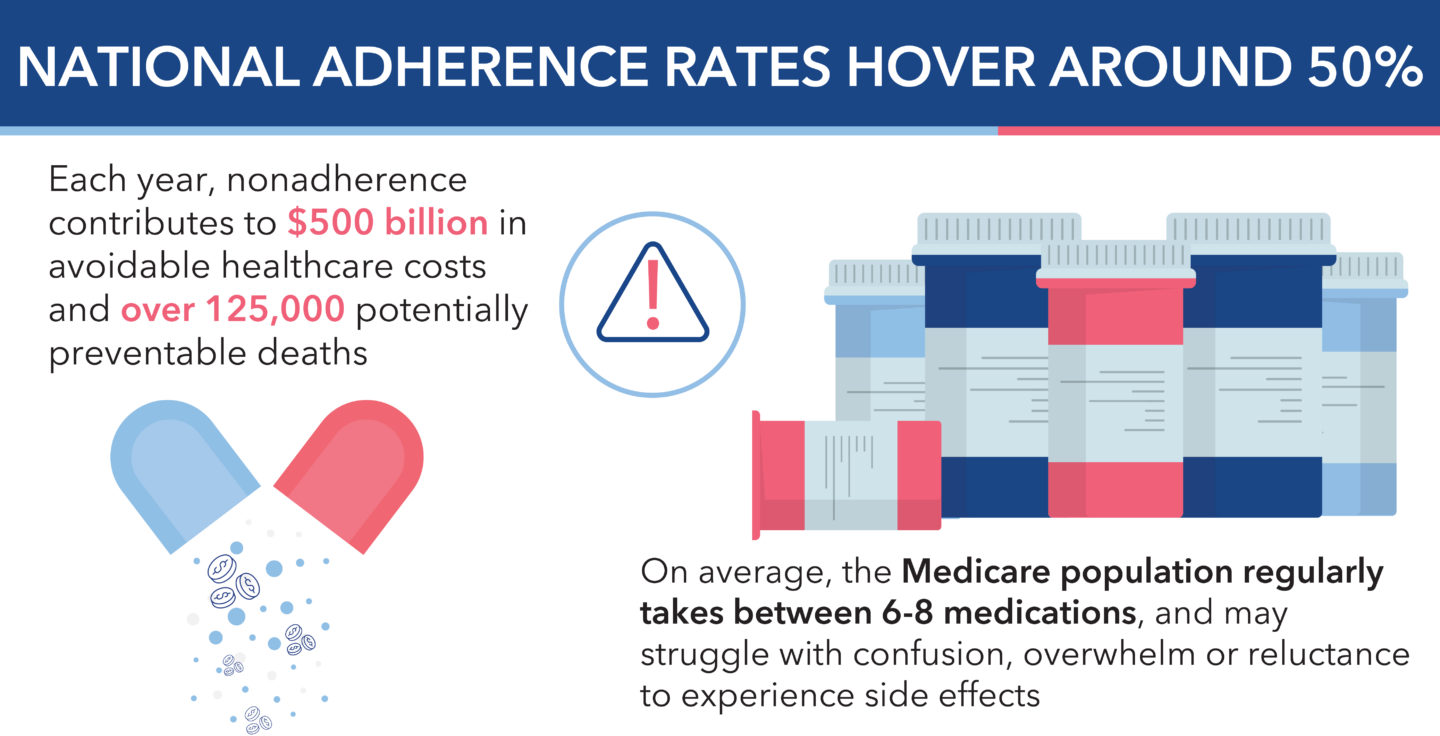
Medication adherence is something that members continue to struggle with, even with the help of traditional health plan strategies. National adherence rates still hover at just around 50%, contributing to $500 billion in avoidable healthcare costs and over 125,000 potentially preventable deaths each year.
MA members face particular difficulties. On average, this population regularly takes between 6 and 8 medications, and may struggle with forgetfulness, confusion, overwhelm or reluctance to experience side effects. All of these challenges may be compounded by functional, cognitive, emotional or socioeconomic barriers.
Achieving 80% PDC
To help members meet or exceed the 80% PDC benchmark, health plans must assess and address challenges members face in maintaining adherence. This begins with leveraging robust data analytics to identify adherence gaps, and proactive outreach that offers tailored interventions. However, a successful strategy must go beyond a one-time interaction to be truly effective.
Medication adherence requires continuous, proactive support that adapts to members’ changing lives throughout each plan year. That’s because adherence requires members to make optimal decisions every single day—often multiple times a day—to take their medications as prescribed. Plans should monitor adherence regularly, identify new obstacles and provide ongoing guidance and resources to help members continually recalibrate when their adherence journey veers off course.
Why a “one-and-done” approach won’t work
There’s a good reason why healthcare stakeholders commonly use the 80% threshold to describe adherence. Consistent access to medications most of the time indicates that members understand the importance of taking their prescriptions, are committed to doing so and are not experiencing ongoing barriers that may prevent them from participating in their own care. However, members are dynamic, changeable, emotional and often unpredictable human beings with a lot on their plates—and medication adherence may not always be their top priority.
For example, members may be prescribed a new medication for a condition they don’t really understand, a change in dosage could produce new side effects that are intolerable to them, or an unexpected expense—medical or otherwise—could threaten their ability to pay for their medicines. Seasonal adherence challenges—like summer travel or holiday disruptions—are also a factor, but barriers to medication adherence are not bound to a seasonal calendar; they evolve day over day, month over month, and year over year.
A member’s ability to adhere to medications can shift due to major life events, such as moving into a new care setting, developing cognitive impairments or facing financial hardship. They may experience a change in living situation or caregiving responsibilities that derails their previous adherence routines. Or they may just start to imperceptibly shift away from good habits as everyday stresses of life take their toll.
Adherence support needs to account for fluctuations such as these, helping ensure members stay on track throughout the year, and beyond.
A year-round approach to medication adherence
To meet adherence requirements, plans must start engaging with members early enough in the year to have an impact. Then, they must maintain a consistent cadence of interactions throughout the next 12-plus months, designed to ensure members don’t dip below the benchmark at any point during the performance period.
A year-round adherence program should include:
An advanced technology platform with data-driven insights into adherence patterns. Digital tools should allow health plans to continuously identify adherence gaps and prioritize members for clinician outreach—including the highest-risk and most complex individuals. The best platforms also include easy-to-use dashboards that help clinicians track interventions throughout the year, and surface key clinical details that boost outreach conversations while helping build member relationships and avoid abrasion that could detract from adherence efforts.
Omnichannel outreach capabilities to reach members by their preferred means. This may include text messaging, email, postal mail and/or phone calls, depending on what resonates best. Members will typically require several touches (often through different channels) before they engage, so plans will need to coordinate activities across channels to maximize engagement without overwhelming members.
Engagement techniques rooted in behavioral science. Trained outreach clinicians should use behavior change strategies proven to promote adherence, including motivational interviewing. This helps better uncover member challenges, to support members and co-produce actionable solutions. These personal, empathetic and collaborative interactions are essential for providing personalized, meaningful adherence support over time.
Care team collaboration. Plans must coordinate with other members of the care team, including prescribers, pharmacies and community-based organizations, to create a holistic support system for members facing adherence risks. Plans should consider reaching out to prescribers and pharmacies to make them aware of member-specific challenges to be addressed. Meanwhile, plans should also form partnerships with community organizations that provide socioeconomic support to quickly and effectively refer members to local resources.
Maximizing the impact of year-round medication adherence activities
Medication adherence is not a one-time effort, but a continuous challenge that evolves with each member’s needs. Plans that rely on single-serve interventions risk losing members at critical points in their health journey.
To maximize the impact of adherence programs, health plans should partner with a vendor that understands the complexities of nonadherence and has the capabilities to provide ongoing, dynamic support. The right partner will use advanced data insights, omnichannel outreach and behavioral science techniques to help members stay on track for the long term.
In conclusion
Improving medication adherence requires a sophisticated, year-round approach that adapts to members’ changing needs. With the right tools and strategies, health plans can improve Star Ratings, reduce costs and help members receive the medications they need, when they need them.
Ready to improve adherence and reduce costs? AdhereHealth specializes in helping health plans navigate these challenges with advanced technology, behavioral science–based engagement and personalized outreach. Contact AdhereHealth today to learn how our proven solutions can help your plan drive year-round medication adherence and better health outcomes.
Want to drive increased member adherence? Learn more in our recent white paper!

Dr. Chandra Y. Osborn
AdhereHealth Chief Experience Officer