Published on .
COVID-19 has amplified the urgency of medication adherence and simultaneously created new obstacles to adherence for high-risk populations, particularly those with challenging social determinants of health (SDOH). Especially during this crisis, an effective medication adherence strategy should focus on addressing the underlying SDOH issues that prevent adherence, such as financial instability and transportation barriers, in order to increase long-term adherence among at-risk consumers. Technology is key to identify, prioritize, and continuously engage with consumers most at risk for non-adherence. When using a technology platform for consumer outreach, it should be equipped to meet four crucial needs: proactive risk-driven outreach to resolve SDOH adherence challenges, data-driven outreach using medical and pharmacy claims to identify non-adherence, a streamlined clinical workflow for smooth consumer engagement and integrated omni-channel provider outreach.
Proactive Risk-Driven Prioritization
When a consumer has difficulty meeting their basic needs, medication adherence drops in priority. COVID-19 has greatly increased the number of people experiencing SDOH limitations like food insecurity or unstable housing with the swift rise in unemployment due to the pandemic. Many high-risk consumers may no longer be able to prioritize their medications as they struggle to meet other life necessities. High-risk consumers with underlying conditions who rely on local or retail pharmacy may encounter obstacles to accessing their medications safely at home.
Throughout this crisis, a tech platform should be equipped to target consumers with risk factors including low-income subsidy, multiple medications, a compromised immune system and people over the age of 50 for proactive outreach and engagement. There are often community resources or health plan benefits in place to help consumers overcome these obstacles, but many consumers are unaware that these resources are available to them without targeted, SDOH-focused outreach.
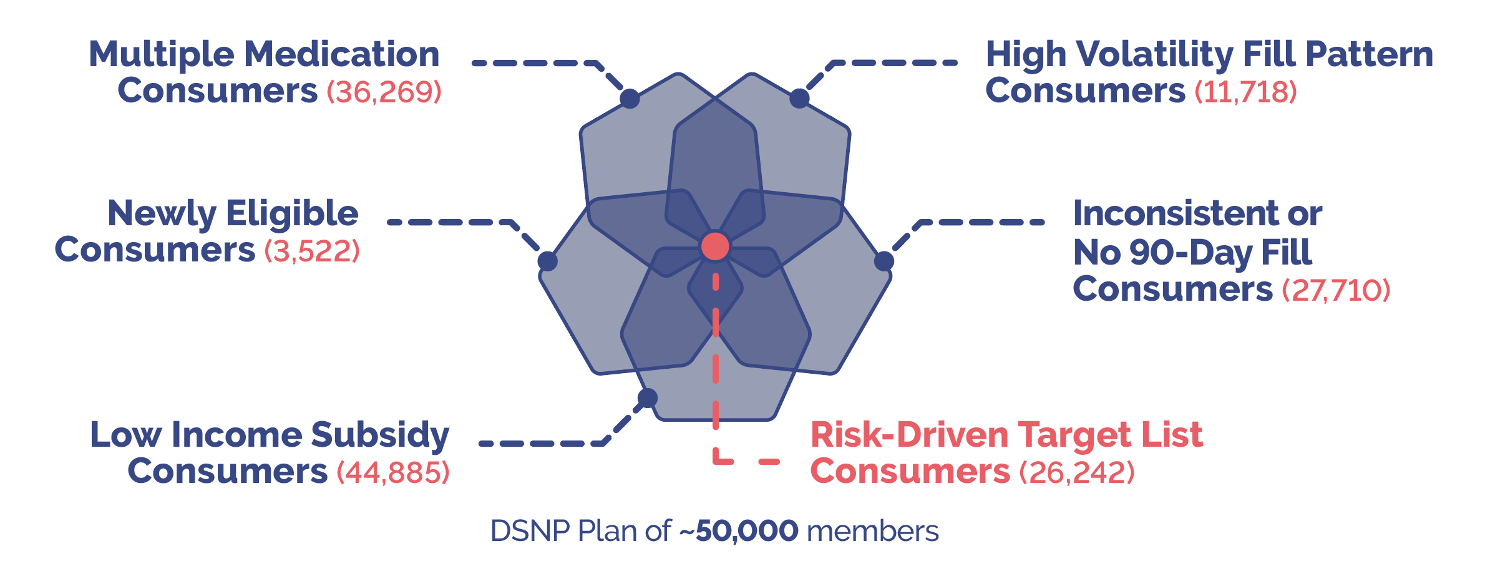
Using predictive analytics, these are the key factors that a technology algorithm should use for prioritization:
Data-Driven Outreach
Along with targeted outreach based on risk factors, a medication adherence tech platform should be able to analyze a comprehensive set of pharmacy and medical claims data in real time to begin outreach as soon as a consumer first skips a refill or is flagged for a drug therapy problem. Real-time data can feed predictive analytics, creating a prioritized outreach queue for clinicians to begin reaching consumers who are most at risk immediately. Utilizing real-time data is especially important in light of COVID-19, when the risks of non-adherence are heightened and some high-risk consumers may be cut off from resources that they typically rely on to access their medications, such as rideshares or caregivers.

A Streamlined Workflow
A consumer experiencing SDOH issues will most likely require multiple engagements to overcome those barriers before a clinician can work with them on becoming adherent. A streamlined workflow is crucial to equipping clinicians to smoothly perform this kind of SDOH-focused meaningful engagement and capture the consumer’s entire journey towards adherence, even if it takes four or five engagements to get there. Each consumer has their own barriers, and a workflow should be built so that clinicians can adapt their approach according to the individual consumer’s needs.
During outreach, clinicians should also be able to immediately connect consumers with community resources or health plan benefits that can help overcome their individual barriers to adherence. With embedded health plan benefit information, a clinician can help a consumer select a lower-price medication or access transportation benefits from their plan. When a clinician can seamlessly connect a consumer to helpful resources, they not only remove barriers to adherence but also establish a trusting relationship so that same consumer will be more receptive to future conversations about adherence.

Integrated Provider Outreach
A lack of care team coordination can contribute to drug therapy problems and prolonged non-adherence in consumers with undetected SDOH issues. Direct provider outreach should be integrated into a medication adherence tech platform to allow clinicians to keep the consumer’s care team informed, especially while consumers may have limited access to their providers due to COVID-19. With omni-channel engagement including telephonic clinician outreach, fax, and EHR, clinicians can reach a provider’s office through their preferred method of contact and alert them to any issues or recommend a reevaluation of their medication regimen if needed.
This direct engagement also allows clinicians to make providers aware of any SDOH factors that may have led to their patient’s non-adherence. People who struggle with SDOH are often reluctant to discuss these issues, especially with a provider, so it frequently takes an empathetic, SDOH-focused approach to uncover them. Once the provider is aware of limitations such as low health literacy or lack of pharmacy access, they can work with the consumer on these issues and improve adherence going forward. Especially while many providers are overloaded due to COVID-19, initiating provider outreach can be a vital touchpoint for at-risk consumers.
Implementing a comprehensive, tech-based approach to medication adherence will benefit high-risk consumers throughout the pandemic and well beyond it. Subscribe to our blog for more COVID-19 and medication adherence related resources
