Published on .
The social determinants of health (SDOH) are inextricably linked to healthcare outcomes. Up to 80% of outcomes are tied to circumstances that directly impact activities of daily living, yet the healthcare system still struggles to adequately identify and address these factors during care delivery. Food insecurity is, unfortunately, the perfect example.
A new USDA report has found that more than 44 million Americans lived in food insecure households in 2022—that’s 10 million more than in 2021—as inflation and other socioeconomic pressures make it more difficult for people to access adequate nutrition. Food is among the most basic of human needs, and people living on extremely tight budgets may be more likely to prioritize the procurement of food over purchases that seem less urgent, like preventive care and maintenance medications.
To address disparities in healthcare and take action on issues such as food insecurity and other SDOH barriers, the Centers for Medicare and Medicaid Services (CMS) has introduced the Health Equity Index (HEI) and Social Needs Screening and Intervention (SNS-E) measures to demand Medicare Advantage (MA) plans improve healthcare access and outcomes for plan members, especially those with specific social risk factors (SRFs).
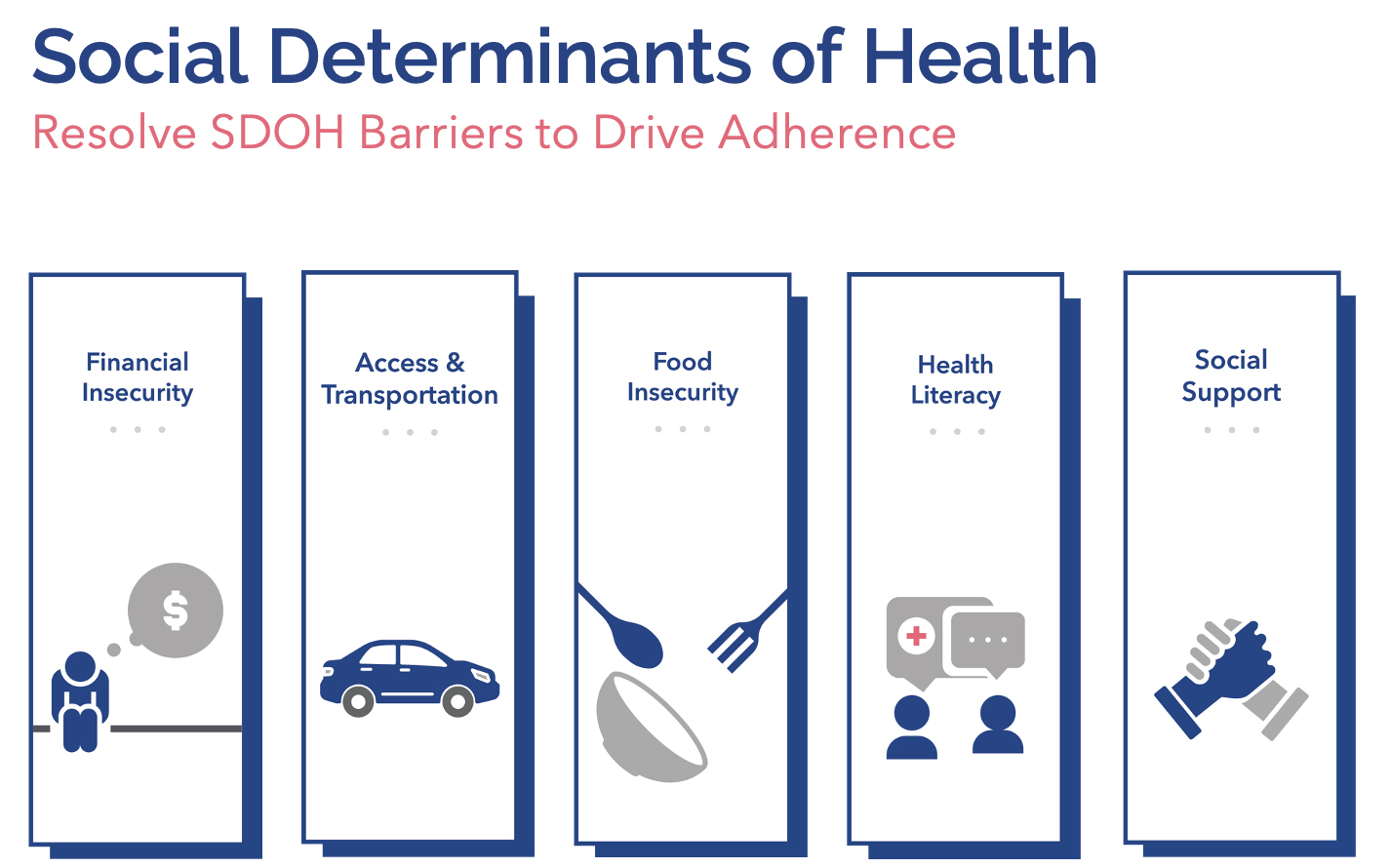
For MA plans, identifying and resolving SDOH barriers, including (but not limited to) food insecurity, can have a major impact on a member’s ability to access necessary care, remain adherent to medications, and achieve more positive outcomes—all of which are also crucial for the success of MA plans in the Star Ratings system.
The link between food insecurity, medication adherence and outcomes
CMS pinned the number of food insecure beneficiaries at 15% in 2021 among Medicare members age 65+, and the Better Medicare Alliance notes that nearly half of the lowest-income Medicare beneficiaries are food insecure, including 48% of MA beneficiaries with incomes less than 100% of the federal poverty line.
One study from 2014 found that “about 28% of [Medicare beneficiaries with diabetes] did not (re)fill any diabetes medication, and over 80% had at least one diabetes complication. Food insecure participants showed comparable (re)fill adherence to food secure participants. However, 57% of food insecure participants were nonadherent to oral hypoglycemics.”
That tracks with overall medication adherence rates from other landmark research. Overall, about half of all chronic disease patients fail to take their medicines as prescribed. For all prescriptions, just 50-70% are picked up, 25-30% are taken as directed, and 15-20% are refilled.1
When food insecure individuals don’t take their medications as prescribed and don’t engage regularly with primary and specialty care, they tend to have worse health outcomes and spend 45% more on healthcare than their food secure peers, according to the Center on Budget and Policy Priorities. After controlling for other SDOH and demographic variables, they found that food insecure people spent an average of $6,100 on medical care per year compared to $4,200 in secure households.
Medicare Advantage plans have an opportunity to change this trajectory by resolving SDOH barriers earlier in the member journey. In turn, this can boost access to prescriptions, reduce the more than 125,000 preventable deaths and over $500 billion in avoidable spending each year associated with improper medication adherence, and improve overall outcomes for the most at-risk members of the community.
How the Star Ratings system is taking on SDOH barriers
The Star Ratings system is undergoing some major changes to hold MA plans accountable for their part in the push for greater health equity. These changes include the introduction of the HEI SNS-E measures.
The HEI will replace the existing reward factor for many plans with a competitive ranking system calculated from existing Stars measures. Using the next two years of data (2024-2025),
eligible plans will be divided into thirds based on their performance: plans in the top third on a given measure will get one point, while plans in the middle get zero and those in the bottom third get a negative point. A positive score is required to qualify for any financial rewards.
Meanwhile, the SNS-E measure will go into effect for 2024 after being a display measure in 2023. Plans will need to submit electronic reporting on the percentage of members who receive standardized screenings for SDOH barriers like unmet food, housing and transportation needs—as well as the percentage of members who receive an applicable intervention if they screen positive for these issues.
High performance on these SDOH-focused requirements can lead to improved overall Star Ratings and enhanced Quality Bonus Program (QBP) payments, in addition to reducing costs of care for the plan through improved health outcomes and reductions in related medical care.
Best practices for addressing SDOH barriers via the Star Ratings system
The HEI and SNS-E measures provide a roadmap for how MA plans can address common SDOH concerns, such as food insecurity. To achieve the dual goals of performing well on Stars while fostering better outcomes for members, plans should consider the following best practices.
Adopt a technology platform to identify at-risk members
The ability to identify at-risk members, and those with SRFs, is the first step toward addressing their needs. MA plans will need to adopt digital tools that use a variety of data sources, including SDOH datasets, to flag members at elevated risk of nonadherence and prioritize these members for outreach.
The most effective platforms should include high-value data visualizations, customizable dashboards and features that recommend the “next best action,” while updating on a daily and weekly basis for near–real-time interventions that reach members at critical points in their healthcare journeys.
Build trust and rapport with members through personalized outreach
Members experiencing food insecurity and other issues may be reluctant to share their challenges with strangers over the phone. Plans will need to use person-centric strategies, such as motivational interviewing, to build trust with members and get to the roots of their medication adherence issues.
To scale up these efforts enough to meet the demands of the HEI and SNS-E measures, plans may need to find a partner that offers access to highly trained, tech-enabled outreach clinicians. When supported by a robust data analytics platform, these engagement specialists are further supported in building rapport with members. Through access to data that provides specific details surfaced through analysis of medical and pharmacy claims, clinicians are able to engage with members on multiple Stars measure requirements during each interaction. This helps maximize outreach efficiency, while minimizing member abrasion.
Provide meaningful interventions and ongoing follow-up
The SNS-E measure will gauge how often members get the tangible help they need to overcome SDOH barriers, such as food insecurity. Using a technology platform that surfaces applicable community resources to the outreach clinician during a member engagement is key for connecting individuals with the right help at the right time.
However, interventions cannot be viewed as a “one-and-done” task. Members facing instability in one area are likely to experience challenges with other basic needs or may dip in and out of at-risk categories due to circumstances beyond their control. Ongoing follow-up conducted at a regular cadence can ensure members continue to have access to the resources they need to stay adherent to their medications, preventive care and other treatments.
This type of consistent outreach and engagement can simultaneously help MA plans meet a variety of important Stars requirements, from the HEI and SNS-E to the triple-weighted medication adherence measures, as well as measures around proactive screenings, member satisfaction and member retention.
Solving for food insecurity and other SDOH barriers – and ensuring that these issues remain under control – is essential for MA plans in the new Star Ratings environment. Plans will need to get to grips with the links between SDOH barriers, spending, and outcomes while employing advanced analytics and person-centered engagement techniques to succeed with upcoming health equity measures while truly making an impact for some of their most vulnerable members.
Learn more about SDOH-focused Stars measures and specific ways to improve adherence and health equity when you join our upcoming webinar on 12/6 at 1 PM CST: Winning with HEI, SNS-E and More: SDOH Strategies Still the Formula for Success
Additional Reference:
- National Association of Chain Drug Stores. Pharmacies: Improving Health, Reducing Costs. July 2010. Based on IMS health data