Published on .
2024 is flying by, with summer on the downswing towards fall. For Medicare Advantage (MA) plans, that means more than half the performance year is already over, and many leaders are already turning their full attention to the new CMS rules and regulations coming next in 2025.
But writing off the remaining days in 2024 could be a costly mistake. The third and fourth quarters aren’t just passive planning periods for the Stars measurement year 2024. Instead, they represent an underutilized opportunity to keep pushing improvements in quality and experiences that could lead to higher Stars performance by the time 2025 rolls around.
A coordinated Q4 push could be especially impactful around CMS HEDIS measure performance, which have an enormous impact on an MA plan’s ability to reach or maintain the critical 4.0+ Star threshold. By using Q4 to close midyear performance gaps around cancer screenings, chronic disease control and care coordination, plans can make the most of every moment and position themselves for even greater success when it does come time to flip the calendar to the new year.
Building momentum with a focus on CMS HEDIS measure performance
Most MA plans make a special effort at the beginning of a new performance period to assess their members for crucial gaps in care so they can check off these yearly activities as soon as possible.
But members don’t always complete preventive care activities on their health plan’s timeline. Members may face social determinants of health (SDOH) barriers, such as low health literacy, that get in the way of access to health services, alongside other access and affordability challenges. Or members may simply have their annual wellness visits scheduled for November instead of March, for example, which could push health maintenance activities into the next year and leave an unintentional gap during the current Stars measurement year 2024.
It helps for plans to routinely analyze care gap patterns and follow up regularly throughout the year—especially close to the end of the measurement year, as time is running out. This last-minute push provides enough time to nudge members into completing important clinical services required for success in HEDIS measures, which can often be checked off quickly.
Reinvigorating outreach in Q4 can lead to significant progress on an important set of HEDIS measures, including measures such as:
- Breast Cancer Screening (BCS)
- Colorectal Cancer Screening (COL)
- Osteoporosis Management in Women who had a Fracture (OMW)
- Eye Exam for Patients with Diabetes (EED)
- Statin Therapy for Patients with Cardiovascular Disease (SPC)
- Social Needs Screening (SNS-E)
- Care for Older Adults (COA): Pain Assessment, Medication Review, Functional Assessment
It pays to make a special effort around these metrics. Because they are set to be the highest-weighted group of Stars measures (now that CMS has reduced the weighting of the CAHPS measures from 4x to 2x), HEDIS measure performance may be the key differentiator that helps plans increase their Star Rating and access the financial incentives that come with 4.0+ Stars.
For example, plans that improve from 3.0 Stars to 4.0 Stars can expect to increase plan revenues between 13.4–17.6 percent through Quality Bonus Program (QBP) incentives and increased enrollment revenue. A one-star bump is correlated with an 8–12 percent increase in enrollment, which could make all the difference for long-term sustainability in an increasingly crowded and highly competitive marketplace.
 Choosing a partner to support a Q4 rally around HEDIS measures
Choosing a partner to support a Q4 rally around HEDIS measures
For the most effective Q4 push, MA plans should consider working with a dedicated partner that has the experience, resources and cutting-edge technology to conduct coordinated outreach to members.
With the right digital platform, including data-driven risk stratification and predictive analytics tools, MA plans can prioritize outreach among the highest-risk, hardest-to-engage plan members, track engagement patterns, and facilitate meaningful, empathetic relationships with members who may be experiencing challenges managing their own health.
Plans aiming for success in Q4 and beyond should look for a partner that takes a comprehensive approach to identifying and closing care gaps. The most effective partners will be able to:
- Understand and execute on an MA plan’s unique Stars strategies and goals. Working closely with plan leaders, a productive partner should have a clear idea of where the plan needs to improve and how to maximize individual and shared resources to achieve goals with measurable results, including leveraging “force multipliers” to raise overall Stars performance.
- Identify opportunities to establish stronger relationships with specific populations. Every MA plan has a cohort of high-spending, medically complex members who are not optimally engaged in their care. Zeroing in on this population using advanced analytics technologies is the first step toward closing HEDIS care gaps, improving overall adherence to care plans and even raising member satisfaction scores.
- Conduct meaningful outreach to connect with high-priority members. Using multichannel communications and proven engagement strategies like motivational interviewing, the ideal partner should be able to connect with members on their terms and encourage participation in health screenings and chronic disease management activities.
- Effectively resolve SDOH barriers. When SDOH concerns get in the way of full engagement in care, the right partner will be able to match members with unused plan benefits and/or provide community referrals to services using an intuitive, workflow-friendly digital platform for managing SDOH-related interactions.
- Provide robust tracking and reporting to measure success. To gauge the impact of the investment, partners should be able to provide comprehensive and detailed reporting on engagement rates, successful interactions, care gaps closed and other metrics that are important for making informed decisions.
A portrait of success with a Q4 push to the finish line
Making smart use of the fourth quarter can have measurable benefits for plans that know every day matters for their members.
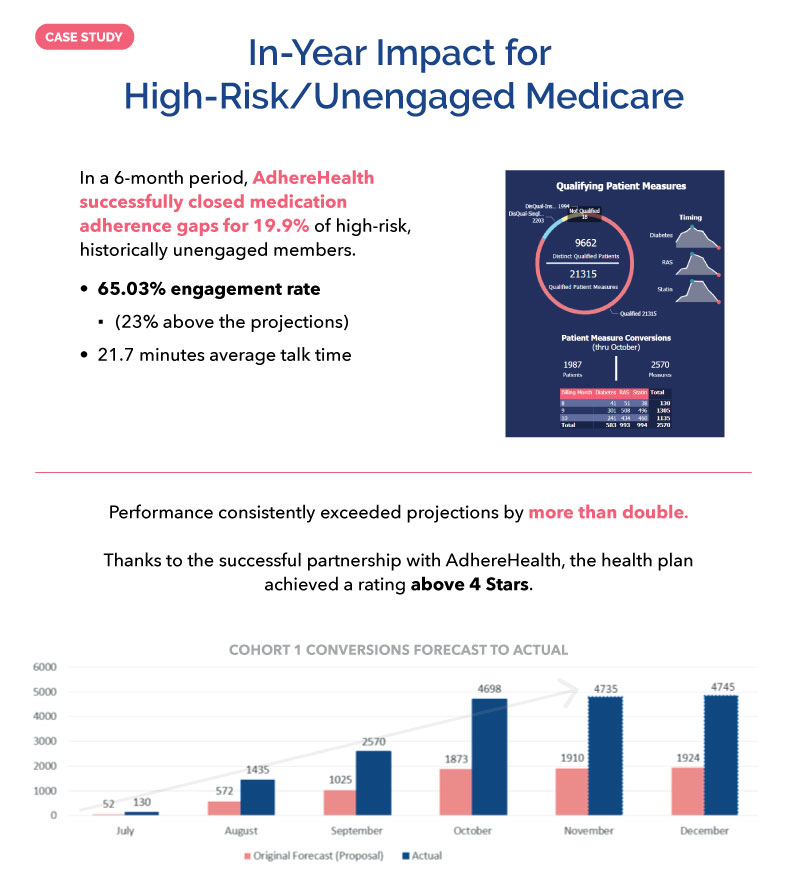
When one national MA plan partnered with AdhereHealth to finish the year strong on behalf of their members, they identified a group of approximately 10,000 people who had not engaged with the health plan in 6 to 18 months.
AdhereHealth’s experienced telepharmacy outreach team leveraged a combination of advanced analytics and personalized communications to reach more than 65% of these individuals in just a few months—a number that was 23% above the projections.
By spending an average of nearly 22 minutes per call with each member, diving deeply into their clinical and non-clinical challenges, the team was able to achieve remarkable results for the members and their plan.
In a 6-month period, with activities concentrated in the last quarter of the year, AdhereHealth was able to successfully close medication adherence gaps for 19.9% of these historically unengaged members, more than doubling projections and assisting the plan with surpassing their Star Ratings goals.
This example shows that it’s never too late to make a difference when it comes to positioning plans for greater success in both the current performance year and the next measurement period.
As the end of the year approaches, it’s not too late for MA plans to harness what’s left of 2024 to close midyear performance gaps and elevate their Star Ratings. A focused push in Q4, particularly around CMS HEDIS measure performance, can significantly boost a plan’s overall Star Rating, as well as access to QBP incentives. By strategically engaging with members and addressing SDOH barriers, plans can make measurable progress.
Partnering with an experienced healthcare technology partner that offers advanced analytics alongside personalized outreach can ensure meaningful connections with members, ultimately driving success. Don’t wait—take action now to secure a strong finish in 2024 and set the stage for an even more successful 2025.
To learn more about how AdhereHealth’s leading-edge technology platform and deep experience in member outreach can help your plan finish 2024 on a high note, contact us today to schedule a consultation.