Published on .
Change is constant in the Medicare Advantage (MA) market. Coming off some transformative adjustments to scoring calculations (e.g., “TukeyGate,” guardrail implementation, etc.), the Star Ratings system is set for additional revamping that will make it even more challenging for MA plans to reach or exceed the critical 4.0-Star threshold.
From a sharper focus on health equity to potentially redesigned methodologies for Medication Therapy Management (MTM) qualification, plus anticipated changes to the QI Hold Harmless Provision and more new measures, proactive plans have long strategic “to-do” lists for the foreseeable future.
But amidst all this change, one thing will remain certain: placing focus on member engagement (especially in high-risk, complex members) as early and often as possible is a key strategy to produce an outsized return on investment. And the yield of this approach is true across the board. From CAHPS measure performance, to HEDIS and medication measures, to universal factors like the Health Equity Index (HEI), successful member engagement is still key to success.
Member engagement is integral to Star Ratings performance
For many plans, “member engagement” initially conjures up thoughts of call center wait times and Net Promoter Scores centered on satisfaction with dispute resolution and payment processing.
While these administrative and operational experiences are certainly important and do have a bearing on Star Ratings via the CAHPS survey, there’s more to fostering relationships that produce truly engaged members—and more opportunities to use these touchpoints to improve Star Ratings outcomes from a clinical and financial perspective.
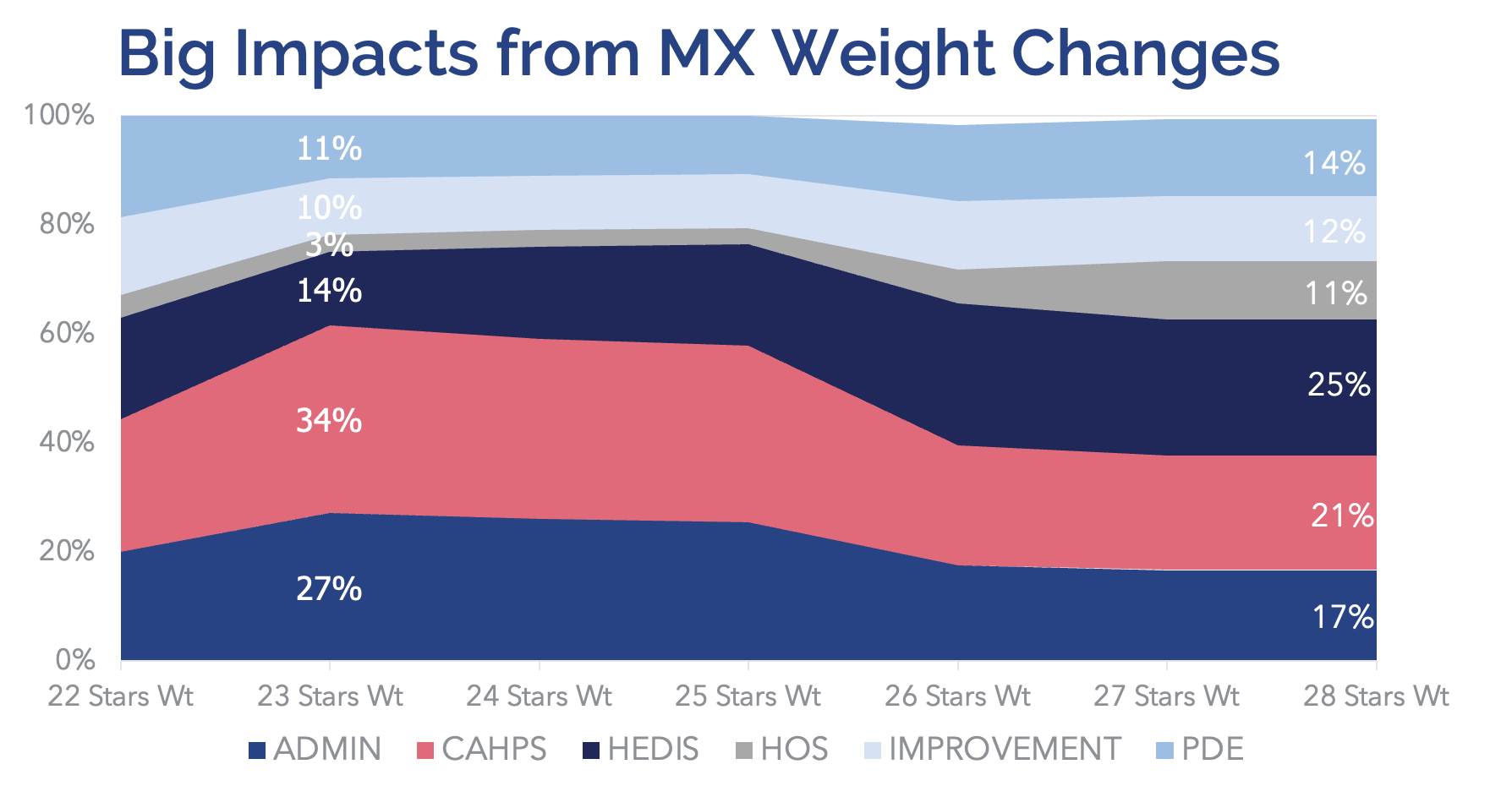
While some plans may be breathing a sigh of relief due to the reduced CAHPS score weighting from 4x to 2x starting in measurement year 2024, it’s not time to shortchange member engagement: CAHPS measures still comprise nine of the Star Ratings measures, so even at a 2x weighting, they’ll have an influence on plans’ overall scores.
 Reference: AdhereHealth webinar 10/11/23, featuring Hyperlift
Reference: AdhereHealth webinar 10/11/23, featuring Hyperlift
Also, there’s still value in supporting positive member experience, because it’s intrinsically linked to measures that are now set to be the highest-weighted group of performance measures: HEDIS. Plans’ efforts towards member engagement are key to performance on these measures because members who are active participants in their care may be more likely to receive preventive care services and make informed decisions about utilization. This can lead to better overall health outcomes, higher satisfaction with their health plan, and reduced medical spending.
In short, when members are satisfied with their plan, they’ll be more likely to take other healthy actions (like attending a wellness exam or getting their flu vaccine), which can result in better Star Ratings performance for health plans on process and adherence measures to improve overall Stars.
CMS finalizes new HEDIS measures
The Healthcare Effectiveness Data and Information Set (HEDIS) helps measure member engagement in a different way by focusing on whether or not important clinical services have been rendered. HEDIS measures include a range of quality metrics, such as blood pressure control, completion of certain cancer screenings, appropriate use of medications for chronic conditions, and transitions of care.
New HEDIS measures that have officially been moved from display measures into the 2024 Star Ratings for the first time include several measures that increase focus on the quality of care related to an inpatient hospital stay to prevent the need for additional emergency care. These include:
- Plan All-Cause Readmissions (PCR)—the percentage of plan members (18 years and older) readmitted to a hospital for the same or a different condition within 30 days after having been released from a hospital stay.
- Transitions of Care (TRC)—the percentage of plan members who received follow-up care after a hospital stay, including information about their health condition and what to do next, having a visit or call with a doctor, and having a doctor or pharmacist make sure the member’s medication records are current.
- Follow-up After Emergency Department Visit for People with Multiple High-Risk Chronic Conditions (FMC)—the percentage of plan members with 2 or more chronic health conditions who received follow-up care within 7 days after an emergency department visit, including a visit with a case manager or other healthcare provider.
 A focus on member engagement is the means to achieving the right ends with HEDIS measures, especially important now as they shift to the heaviest weighted group within the Star Ratings lineup. Proactive health plans can incentivize the right preventive and maintenance care at the right time by informing members of clinical recommendations and ensuring they have the tools and support to complete screenings and other services in a timely manner. Given the influence of Tukey to raise measure cut points to record highs, plans must put focus on performance on HEDIS measures to remain competitive on the path to 4.0+ Stars.
A focus on member engagement is the means to achieving the right ends with HEDIS measures, especially important now as they shift to the heaviest weighted group within the Star Ratings lineup. Proactive health plans can incentivize the right preventive and maintenance care at the right time by informing members of clinical recommendations and ensuring they have the tools and support to complete screenings and other services in a timely manner. Given the influence of Tukey to raise measure cut points to record highs, plans must put focus on performance on HEDIS measures to remain competitive on the path to 4.0+ Stars.
What does an evolving member engagement environment mean for MA plans?
To support positive member engagement, holistic approaches to building and maintaining strong engagement and trusted relationships with members are helpful to avoid member abrasion that can erode engagement efforts. Leaders will need to focus on the fulcrum points for activating members and achieving long-term results with outcomes and spending.
The goal is to treat HEDIS measures as more than a “one-and-done” lift. Instead, plans will need to build an ongoing cadence of touchpoints and check-ins for members that keep outreach comprehensive and integrated, and address member healthcare needs. This is particularly important in the chronically unengaged, and helps plans maintain positive results over time and keep Star Ratings high, year after year. A case example would be having access to data that prompts outreach to a diabetic member after discharge from the hospital, but that also reveals the member has high blood pressure. This allows an outreach clinician to connect with the member on multiple touch points during the same call that impact the member’s overall health and help the plan meet requirements for related Stars measures.
The most effective strategies take full advantage of every interaction with the member by ensuring that outreach staff have a complete record of the member’s care gaps, recent activities and socioeconomic barriers at their fingertips. By equipping staff with timely and accurate information, plans can accomplish more with less abrasion to members, especially those that are hard to reach or are resistant to participating.
Best practices for creating and sustaining holistic member engagement
Partnerships, technologies and creativity all play a significant role in a health plan’s success with improving their member relationships. Plans should consider the entire flow of engagement—from identifying potential barriers, to obtaining critical health care services, to forming relationships with members and following up on care gaps with specific documented action steps. This end-to-end approach helps ensure all activities are well-coordinated with minimal back-and-forth that could lose members along the way.
Use technology to identify high-risk, unengaged members
The right data analytics platform can aggregate and analyze multiple data sources, including clinical, claims, pharmacy and SDOH data, to flag members with complex health issues, existing gaps in care, or underlying risks of disease exacerbation. By prioritizing these members for targeted outreach, plans can cover more ground with fewer resources and see a rapid boost to their Star Ratings performance.
To maximize results, this data should be intuitively available as integrated decision support for outreach staff within a seamless workflow, so staff can feel confident in their recommendations and members don’t have to repeat themselves.
Support members with resolving SDOH barriers
Socioeconomic challenges, such as lack of transportation or financial insecurity, can quickly lead to poor medication adherence, lack of access to care services, inappropriate care utilization, and an escalation of undesirable health outcomes. With new universal initiatives like the Health Equity Index (HEI) measure, MA plans are becoming more and more responsible for identifying and resolving these issues before they start to interfere with care.
Plans might consider bringing in a partner with expertise in uncovering and learning about SDOH barriers through motivational interviewing and other person-centered strategies to make sure every member feels comfortable talking about their needs.
After identifying the issues, however, plans must go one step further and assist members with connection to community-based resources or plan benefits that can resolve their concerns. With fewer barriers to care, members are more likely to remain adherent to their medications, complete recommended services, and avoid unnecessary spending on ED visits or unplanned readmissions.
Turn process measures into a companion to better outcomes
Member engagement drives positive results, but high-risk members can be difficult to engage because they’re often difficult to reach. For that reason, treating faster-to-resolve HEDIS process measures as a “companion” to more longitudinal measures of success (such as the adherence measures around RAS, statin and diabetes medications) helps improve Star Ratings performance across the board.
Longitudinal measures require engagement over time (at least 80% of the year to reach the percentage of days covered [PDC] threshold) and are a strong indicator of success with establishing and maintaining member relationships. However, both types of measures must be addressed in conjunction to achieve results, which may put the squeeze on health plans that don’t have help with the resources and techniques to get it done.
Plans may wish to bring in a partner with the dedicated peoplepower and advanced technology to manage the engagements required to ensure nothing slips through the cracks, but without overloading members with phone calls or messages.
Getting Ahead of Star Ratings Improvements with a Holistic Engagement Strategy
There is still time in the 2023 measurement year to set the stage for improved Star Ratings and prepare for proposed changes due to begin over the next few years. Q4 is the perfect time to launch an intensive campaign to prime higher-risk members for engagement in Q1 and beyond. By focusing on member engagement now and implementing a more holistic strategy to tackle HEDIS measure performance, MA plans can navigate changes to the Star Ratings system and position themselves for long-term success in a rapidly evolving environment.
Looking to get a foothold on your MA plan’s Star Ratings? Register for the second webinar in our 3-part series as our panelists dive deep into 2024 Star Ratings results: Transforming Stars Scoring Shockwaves: Pivotal Strategies for Positive Impact. Register today!
Authored by:
Kempton Presley
Chief Analytics Officer at AdhereHealth

